DEPARTMENT OF HEALTH AND SOCIAL SERVICES
Division of Medicaid and Medical Assistance
FINAL
ORDER
Medicaid Recovery Audit Contractors Program
REVISION OF THE REGULATION |
OF DELAWARE'S |
TITLE XIX MEDICAID STATE PLAN |
SECTION 4.5 GENERAL PROGRAM |
ADMINISTRATION PAGES 36, 36A, AND 36B |
NATURE OF THE PROCEEDINGS:
Delaware Health and Social Services ("Department") / Division of Medicaid and Medical Assistance initiated proceedings to amend Title XIX Medicaid State Plan regarding the Medicaid Recovery Audit Contractor (RAC) Program, specifically, to request an exception to the RAC contracting requirements. The Department's proceedings to amend its regulations were initiated pursuant to 29 Delaware Code Section 10114 and its authority as prescribed by 31 Delaware Code Section 512.
The Department published its notice of proposed regulation changes pursuant to 29 Delaware Code Section 10115 in the July 2018 Delaware Register of Regulations, requiring written materials and suggestions from the public concerning the proposed regulations to be produced by July 31, 2018 at which time the Department would receive information, factual evidence and public comment to the said proposed changes to the regulations.
SUMMARY OF PROPOSAL
Effective for services provided on and after July 1, 2018 Delaware Health and Social Services/ Division of Medicaid and Medical Assistance proposes to amend Section 4.5 General Program Administration Pages 36, 36a, and 36b of Title XIX Medicaid State Plan regarding the Medicaid Recovery Audit Contractor (RAC) Program, specifically, to request an exception to the RAC contracting requirements.
Background
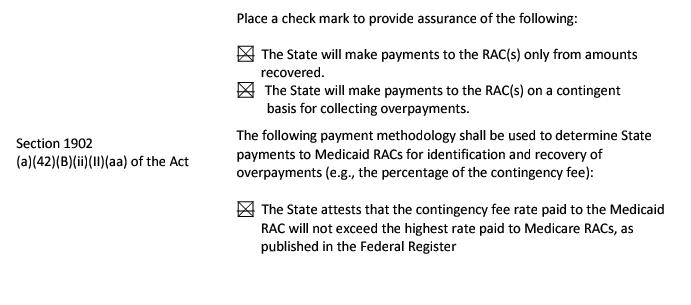
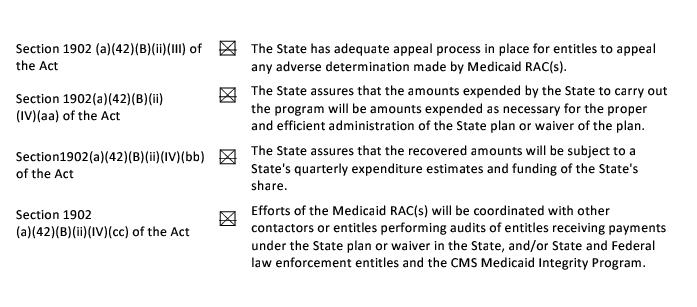
Under Section 1902(a)(42)(B)(i) of the Act, states and territories are required to establish programs to contract with one or more Medicaid Recovery Audit Contractors (RACs) for the purpose of identifying underpayments and overpayments, as well as recouping overpayments, under the Medicaid State Plan and any Medicaid State Plan Waivers. This applies to all services for which payment is made to any entity under such plan or waiver. States must establish these programs in a manner consistent with State law, and generally in the same manner as the Secretary contracts with contingency fee contractors for the Medicare RAC program.
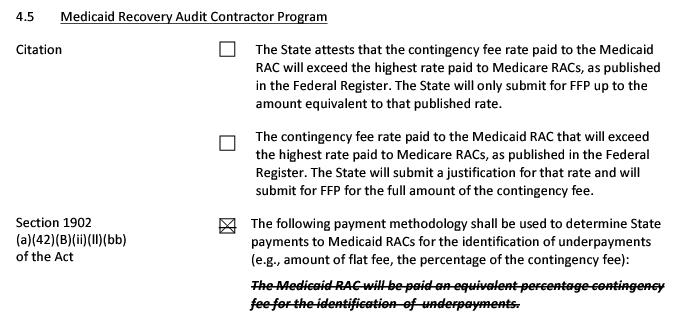
Section 1902(a)(42)(B)(i) of the Act specifies that States shall establish programs under which they contract with Medicaid RACs subject to such exceptions or requirements as the Secretary may require for purposes of a particular State. This provision enables the Centers for Medicare and Medicaid Services (CMS) to vary the Medicaid RAC program requirements. For example, CMS may exempt a State from the requirement to pay Medicaid RACs on a contingent basis for collecting overpayments when State law expressly prohibits contingency fee contracting. However, some other fee structure could be required under any such exception (e.g., a flat fee arrangement).
States that otherwise wish to request variances with respect to, or an exception from, Medicaid RAC program requirements must submit a request to CMS, in writing, from the State's Medicaid Director to the CMS/Medicaid Integrity Group.
Although the Delaware Division of Medicaid and Medical Assistance (DMMA) previously had a Recovery Audit Contract (RAC) vendor, that contract is no longer in place. DMMA posted a Request for Proposals (RFPs) in an attempt to attract a new RAC vendor, but received no bids. The majority of Delaware's Medicaid population is enrolled in managed care and the providers treating them are not subject to audit recovery contracting. There is not sufficient revenue generation to fund an adequate contingency fee.
Statutory Authority
Purpose
Purpose
The purpose of this proposed regulation is to seek an exception to the RAC contracting requirements.
Summary of Proposed Changes
Effective for services provided on and after July 1, 2018 Delaware Health and Social Services/Division of Medicaid and Medical Assistance (DHSS/DMMA) proposes to amend Section 4.5 General Program Administration Pages 36, 36a, and 36b of Title XIX Medicaid State Plan regarding the Medicaid Recovery Audit Contractor (RAC) Program, specifically, to request an exception to the RAC contracting requirements.
Public Notice
In accordance with the federal public notice requirements established at Section 1902(a)(13)(A) of the Social Security Act and 42 CFR 447.205 and the state public notice requirements of Title 29, Chapter 101 of the Delaware Code, Delaware Health and Social Services (DHSS)/Division of Medicaid and Medical Assistance (DMMA) gives public notice and provides an open comment period for thirty (30) days to allow all stakeholders an opportunity to provide input on the proposed regulation. Comments were to have been received by 4:30 p.m. on July 31, 2018.
Centers for Medicare and Medicaid Services Review and Approval
The provisions of this state plan amendment (SPA) are subject to approval by the Centers for Medicare and Medicaid Services (CMS). The draft SPA page(s) may undergo further revisions before and after submittal to CMS based upon public comment and/or CMS feedback. The final version may be subject to significant change.
Provider Manuals and Communications Update
Also, there may be additional provider manuals that may require updates as a result of these changes. The applicable Delaware Medical Assistance Program (DMAP) Provider Policy Specific Manuals and/or Delaware Medical Assistance Portal will be updated. Manual updates, revised pages or additions to the provider manual are issued, as required, for new policy, policy clarification, and/or revisions to the DMAP program. Provider billing guidelines or instructions to incorporate any new requirement may also be issued. A newsletter system is utilized to distribute new or revised manual material and to provide any other pertinent information regarding DMAP updates. DMAP updates are available on the Delaware Medical Assistance Portal website: https://medicaid.dhss.delaware.gov/provider
Fiscal Impact Statement
The proposed amendment is being implemented to clarify current DMMA practices and does not result in a change in current practice. Therefore, there is no projected fiscal impact.
Summary of Comments Received with Agency Response and Explanation of Changes
No public comments were received during the public comment period.
FINDINGS OF FACT:
The Department finds that the proposed changes as set forth in the July 2018 Register of Regulations should be adopted.
THEREFORE, IT IS ORDERED, that the proposed regulation to amend Title XIX Medicaid State Plan regarding the Medicaid Recovery Audit Contractor (RAC) Program, specifically, to request an exception to the RAC contracting requirements, is adopted and shall be final effective September 12, 2018.
8/17/18
Kara Odom Walker, MD, MPH, MSHS
Secretary, DHSS
FINAL
Revision: HCFA-PM-88-10 (BERC) OMB No: 0938-0193
September 1988 36
FINAL STATE PLAN UNDER TITLE XIX OF THE SOCIAL SECURITY ACT
STATE/TERRITORY: DELAWARE
Citation
42 CFR 455.12 4.5 Medicaid Agency Fraud Detection and Investigation Program
AT 78 90
48 FR 3742 The Medicaid agency has established and will maintain
52 FR 48817 methods, criteria, and procedures that will meet all
§1902(a)(42)(B) requirements of 42 CFR 455.13 through 455.21 and 455.23
P.L. 111-148 for prevention and control of program fraud and abuse,
§42 CFR 455 Subpart A including methods for identification, investigation, and
§42 CFR 455 Subpart F referral of suspected fraud cases.
|
TN No. SPA# 18-002
Supersedes HCFA ID: 1010P/0012P
TN No. SP# 268
|
Approval Date
Effective Date July 1, 2018
|
FINAL
36a
STATE PLAN UNDER TITLE XIX OF THE SOCIAL SECURITY ACT
STATE/TERRITORY: DELAWARE
4.5 Medicaid Recovery Audit Contractor Program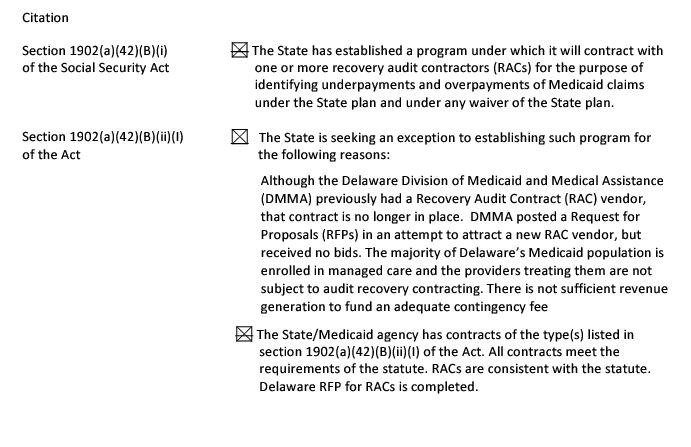
TN No. SPA# 18-002 Supersedes TN No. 10-005 | Approval Date __________ Effective Date July 1, 2018 |
FINAL
36b
STATE PLAN UNDER TITLE XIX OF THE SOCIAL SECURITY ACT
STATE/TERRITORY: DELAWARE
TN No. SPA# 18-002 Supersedes TN No. 10-005 | Approval Date Effective Date July 1, 2018 |







