DEPARTMENT OF HEALTH AND SOCIAL SERVICES
Division of Public Health
PROPOSED
PUBLIC NOTICE
4304 Medical Orders for Life-Sustaining Treatment or Pre-Hospital Advance Care Directives
Division of Public Health, Department of Health and Social Services, is proposing to repeal and replace regulations for Delaware Medical Orders Scope of Treatment (DMOST). The purpose of replacing existing regulation with the proposed regulations is to improve the quality of care people receive at the end of life by translating patient/resident goals and preferences into medical orders. The proposed regulations will set requirements for use of DMOST forms, provide guidance in the use of the forms and formalize the DMOST form itself. On November 1, 2015, DPH plans to publish as proposed the new regulations, and hold them out for public comment per Delaware law.
NOTICE OF PUBLIC COMMENT PERIOD
Copies of the proposed regulations are available for review in the November 1, 2015 edition of the Delaware Register of Regulations, accessible online at: http://regulations.delaware.gov or by calling the Division of Public Health at (302) 744-4951.
Any person who wishes to make written suggestions, testimony, briefs or other written materials concerning the proposed regulations must submit same to Jamie Mack by Friday, December 4, 2015, at:
Jamie Mack
Division of Public Health
417 Federal Street
Dover, DE 19901
Email: jamie.mack@state.de.us
Phone: (302) 744-4951
4304 Medical Orders for Life-Sustaining Treatment or Pre-Hospital Advance Care Directives
Purpose: There is a need to update the existing 2003 Pre-Hospital Advance Care Directive (???PACD???) regulations (7 Del. Reg. 85, July 1, 2003) to address the recognition of advance care directives across all health care settings, including, but not limited to, hospitals, long-term care facilities, hospices, emergency medical transport, and home care. As provided in Chapter 25 of Title 16 of the Delaware Code, advance care directives permit individuals to give instructions about their own health care in case they later lack the capacity to do so.
These regulations require the use of a designated form which can be readily recognized and verified during an emergency situation. Since the creation of the PACD form, the practice and use of similar forms has evolved in states across the country. The Medical Orders for Life-Sustaining Treatment (???MOLST???) form reflects the dominant national trend and is being adopted as an updated version of the PACD form.
Delaware???s current PACD loses its authority when a patient changes locations. Patients at the end of life often move from home to hospital to nursing home and with each move, forms and orders must be redone.
Emergency medical services (EMS) personnel work under the license of the State EMS Medical Director. In order for EMS personnel to honor an individual???s request related to end of life decisions, the EMS must have a medical order. The MOLST form serves both as the summary of the individual???s advance care planning decisions and as the medical order.
Living wills, power of attorney and other advance directives have material limitations. They are often long and complex, can vary greatly in form and content, are subject to various interpretations, and do not constitute a medical order. Many are hand-written and are impossible to verify on the scene of an emergency. In contrast, a Delaware MOLST is a specific order set initiated by the individual and signed by a physician or other authorized health care professional stipulating a specific order set for scope of medical treatment.
These MOLST/PACD regulations authorize the Division of Public Health/Office of Emergency Medical Services in conjunction with the Board of Medical Licensure and Discipline, the Delaware Fire Prevention Commission, and other key groups within the State to develop and implement MOLST/PACD protocol. These regulations, protocol, and form standardize the legal advance care directive documentation so that EMS and all health care providers have a readily recognizable form which sets forth the patients??? preferences regarding provision of life-sustaining treatments. The MOLST/PACD forms allow EMS and other health care providers both to identify and to honor an individual???s wishes to the greatest extent possible and to grant individuals the dignity, humanity, and compassion they deserve. Consistent with this intent, other health care providers may choose to honor this form. (Delaware MOLST, Medical Orders for Life-Sustaining Treatment, form is available in PDF format).
???Advance Health Care Directive??? shall mean an individual instruction or power of attorney for health care, or both.
???Agent??? shall mean an individual designated as power of attorney for health care to make a health care decisions for the individual granting the power.
???Artificial Nutrition And Hydration??? means supplying food and water through a conduit, such as a tube or intravenous line where the recipient is not required to chew or swallow voluntarily, including, but not limited to, nasogastric tubes, gastrostomies, jejunostomies and intravenous infusions. Artificial nutrition and hydration does not include assisted feeding, such as spoon or bottle-feeding.
???Capacity??? shall mean an individual???s ability to understand the significant benefits, risks and alternatives to proposed health care and to make and communicate a health care decision.
???Declarant??? shall mean an individual who executes an advance health care directive.
???Division??? shall mean the Division of Public Health.
???DNR??? shall mean Do Not Resuscitate.
???Emergency Medical Services (EMS) Provider??? shall mean individual providers certified by the Delaware State Fire Commission or the Office of Emergency Medical Services, within the Division of Public Health, Department of Health and Social Services or emergency certified medical dispatchers by the National Academy of Emergency Medical Dispatch.
???Emergency Medical Services (EMS) Provider Agency??? shall mean a provider agency certified by the Delaware State Fire Prevention Commission or the Office of Emergency Medical Services, or an emergency medical dispatch center under contract with the Department of Public Safety.
???EMS Prehospital Advanced Care Directive Order (PACD)??? shall mean an advanced health care directive signed by the individual???s physician on forms approved by the Director of the Division of Public Health.
???EMS PACD Program??? shall mean the regulations and administrative guidelines promulgated by the Division of Public Health for the administration of this Act.
???Guardian??? shall mean a judicially appointed guardian or conservator having authority to make health care decisions for an individual.
???Health Care??? shall mean any care, treatment, service or procedure to maintain, diagnose or otherwise affect an individual???s physical or mental condition.
???Health Care Decision??? shall mean a decision made by an individual or the individual???s agent, surrogate or guardian regarding the individual???s health care, including:
1. Selection and discharge of health care providers and institutions;
2. Acceptance or refusal of diagnostic tests, surgical procedures, programs of medication resuscitation; and
3. Directions to provide, withhold or withdraw artificial nutrition and hydration and all other forms of health care.
???Health Care Institution??? means an institution, facility or agency licensed, certified or otherwise authorized or permitted by law to provide health care in the ordinary course of business or practice of profession.
???Individual??? means an individual person, legally adult.
???Individual Instruction??? means an individual???s direction concerning a health-care decision for the individual.
???Life-sustaining Procedure??? means
1. Any medical procedure, treatment or intervention that:
a. Utilizes mechanical or other artificial means to sustain, restore, or supplant a spontaneous vital function; and
b. Is of such a nature as to afford an individual no reasonable expectation of recovery from a terminal condition or permanent unconsciousness.
2. Procedures that can include, but are not limited to, assisted ventilation, renal dialysis, surgical procedures, blood transfusions and the administration of drugs, antibiotics and artificial nutrition and hydration.
???Medical Orders for Life-Sustaining Treatment??? (???MOLST???) means a specific order set for scope of medical treatment and provided on the MOLST form approved by the Division of Public Health.
???Medically Ineffective Treatment??? means that, to a reasonable degree of medical certainty, a medical procedure will not:
1. Prevent or reduce the deterioration of the health of an individual: or
2. Prevent the impending death of an individual.
???Office??? shall mean the Office of Emergency Medical Services (EMS) within the Division of Public Health.
"PACD" means an EMS prehospital advanced care directive signed by the individual and the individual???s physician, on forms approved by the Director of Public Health.
???Permanent Unconsciousness??? means a medical condition that has existed for at least 4 weeks and that has been diagnosed in accordance with currently accepted medical standards and with reasonable medical certainty as total and irreversible loss of consciousness and capacity for interaction with the environment. The term includes, without limitation, a persistent vegetative state or irreversible coma. This condition must be certified in writing in the patient's medical record by the attending physician and by at least 1 other physician who shall be a board-certified neurologist and/or neurosurgeon.
???Physician??? means an individual licensed to practice medicine under Chapter 17 of Title 24 of the Delaware Code.
???Power Of Attorney For Health Care??? means the designation of an agent to make health care decisions for the individual granting the power.
???Primary Physician??? or ???Attending Physician??? shall mean a physician designated by an individual or the individual???s agent, surrogate or guardian to have primary responsibility for the individual???s health care or, in the absence of a designation, or if the designated physician is not reasonably available, a physician who undertakes the responsibility for the individual???s health care.
???Reasonably Available??? shall mean readily able to be contacted without undue effort and willing and able to act in a timely manner considering the urgency of the individual???s health care needs.
???Supervising Health Care Provider or Health Care Provider??? shall mean the primary physician, or if there is no primary physician or the primary physician is not reasonably available, the health care provider who has undertaken primary responsibility for an individual???s health care.
???Surrogate??? means an adult individual or individuals who (1) have capacity; (2) are reasonably available; (3) are willing to make health care decisions, including decisions to initiate, refuse to initiate, continue or discontinue the use of a life sustaining procedure on behalf of a patient who lacks capacity; and (4) are identified by the attending physician in accordance with 16 Del.C. ??2507 as the person or persons who are to make those decisions.
???Terminal Condition??? means any disease, illness or condition sustained by any human being for which there is no reasonable medical expectation of recovery and which, as a medical probability will result in the death of such human being regardless of the use or discontinuance of medical treatment implemented for the purpose of sustaining life or the life processes.
2.1 An individual, legally adult, who is mentally competent, has the right to refuse medical or surgical treatment if such refusal is not contrary to existing public health laws.
3.1 Any individual with legal capacity may execute a Medical Order for Life-Sustaining Treatment (MOLST) or a Pre-Hospital Advanced Care Directive (PACD); however, this Directive will not become effective unless, after diagnosis of a terminal condition, or a determination of permanent unconsciousness, it is signed by a physician or other health care provider permitted by state law.
3.2 An individual with legal capacity, who is able to communicate by some reliable, proven means (e.g., verbalization, eye blink, finger tap) but is physically unable to sign, may execute a MOLST or PACD through an agent, surrogate, or guardian. Conditions that may prevent physical signing of a MOLST or the PACD include, but are not limited to:
3.2.1 Blindness or illiteracy
3.2.2 Severe arthritis
3.2.3 Amyotrophic lateral sclerosis (ALS or Lou Gehrig???s disease)
3.2.4 Quadriplegia
3.2.5 Paralysis of the writing hand
3.2.6 Amputation
3.3 An individual who no longer has capacity may be issued a MOLST or PACD through an agent, guardian or surrogate and the individual???s physician or authorized health care provider.
3.3.1 Conditions for which a MOLST or PACD may be issued are:
3.3.1.1 Terminal Condition
3.3.1.2 Permanent Unconciousness
4.1 Medical Orders for Life-Sustaining Treatment may contain the following options
4.1.1 Cardiopulmonary Resuscitation or No Cardiopulmonary Resuscitation (If person has no pulse and is not breathing)
4.1.2 Medical Interventions (If person has a pulse and/or is breathing.)
4.1.2.1 Comfort Measures Only (The use of medications by any route, positioning, wound care, and other measures to relieve pain and suffering. Use of oxygen, oral suctioning and manual treatment of airway obstruction as needed for comfort. Do not transfer to the hospital for life-sustaining treatment. Transfer if comfort needs cannot be met in current location).
4.1.2.2 Limited Additional Interventions. (Includes care described above, IV fluids, and cardiac monitoring as indicated. Do not use intubation or mechanical ventilations. May use non-invasive airway support, [e.g. CPAP, BIPAP]. Transfer to hospital, if indicated.)
4.1.2.3 Full treatment. (Includes care described above, use of intubation, advanced airway interventions, mechanical ventilation, and cardioversion, as indicated. Transfer to hospital, if indicated. Includes intensive care, Additional orders [e.g. dialysis, etc.])
4.1.2.4 Antibiotics
4.1.2.4.1 No antibiotics. Use other measures to relieve symptoms.
4.1.2.4.2 Limited use of antibiotics to provide comfort.
4.1.2.4.3 Use antibiotics to prolong life. (Additional Orders:)
4.1.2.5 Artificially administered nutrition: (Always offer food and liquids by mouth, if feasible.)
4.1.2.5.1 No artificial nutrition by tube.
4.1.2.5.2 Defined trial period of artificial nutrition by tube. (Goal:)
4.1.2.5.3 Long-term artificial nutrition by tube. (Additional orders:)
5.1 Prehospital Advanced Care Directives Options
5.1.1 Option A (Advanced Life Support) - ???Maximal (Restorative) Care Before Arrest, Then DNR???
5.1.1.1 When this option is selected on an EMS PACD, the individual shall receive the full scope of restorative interventions permissible under the Delaware Statewide ALS treatment protocol (including intubation for respiratory distress, cardiac monitoring, synchronized cardioversion for pulse-present ventricular or supra ventricular tachycardia, cardiac pacing for pulse-present symptomatic bradycardia, insertion of IV???s, and drug therapy), in an attempt to forestall cardiac or respiratory arrest (see Delaware Statewide ALS treatment protocol for full description of permissible interventions).
5.1.2 Option B (Basic Life Support) ??? ???Limited (Palliative) Care Only Before Arrest, Then DNR???
5.1.2.1 Palliative care is defined as supportive care for control of signs and symptoms.
5.1.2.1.1 This includes opening the airway using non-invasive means (e.g. chin lift, jaw thrust, finger sweep, nasopharyngeal airway, oropharyngeal airway and abdominal thrust, O2 administration, suctioning, positioning for comfort, control of external bleeding using standard treatments (dressing, elevation, direct pressure, pressure points, cold packs, tourniquets, etc.), immobilizing fractures, and family or other health care provider administered medications for pain control.
5.1.2.1.2 Existing IV lines may be in place and, if so, shall be monitored to the extent possible according to the provider???s level of certification and licensure.
5.1.2.2 Inappropriate Care for a Palliative Care Individual includes:
5.1.2.2.1 Pacing, cardioversion, and defibrillation
5.1.2.2.2 Initiation of IV therapy
5.1.2.2.3 EMS Initiated Medications - Except passive oxygen
5.1.2.2.4 CPR
5.1.2.2.5 Intubation (EOA, endotracheal, nasotracheal, or gastric tube)
5.1.2.2.6 Pneumatic anti-shock garment (PASG)
5.1.2.2.7 Active ventilatory assistance, unless on an out individual ventilator.
5.1.3 Option C (Do Not Resuscitate) ???No Care Administered Of Any Kind???.
5.1.3.1 This option permits an individual to reject care of any kind provided there is a signed order clearly stating this course of action. Where this option is in place, no form of life saving efforts, including but not limited to, the opening of the airway, the administration of oxygen, or any other form of life-saving efforts will be administered by EMS personnel under any circumstances, unless the individual provides some form of communication as indicated in Section 3.2.
5.1.4 Nothing in this regulation will require an EMS provider to comply with a Pre-Hospital Advanced Care Directive for reasons of conscience.
6.1 Provided there is a signed MOLST, PACD, or other approved Division of Public Health signed form, the following are acceptable for implementing methods to identify to the EMS the existence of a MOLST or PACD form and to implement the MOLST/PACD protocol:
6.1.1 Delaware MOLST or EMS PACD Fform
6.1.2 Delaware MOLST or EMS PACD Wallet Card
6.1.3 Delaware MOLST Wrist Bracelet to include Medic-Alert Bracelet or other bracelet approved by the Director of the Division of Public Health.
6.1.4 Other State EMS PACD or MOLST Form
6.2 Even if a signed PACD, MOLST, or other approved Division of Public Health signed form is present, the following are not acceptable for implementing the EMS PACD or MOLST protocol:
6.2.1 Advance directives without an EMS PACD or MOLST form
6.2.2 Facility specific PACDs DNR forms
6.2.3 Notes in medical records
6.2.4 Prescription pad orders
6.2.5 PACD stickers
6.2.6 Any oral request.
6.2.7 Any other device or instrument not listed above as acceptable.
6.3 The Delaware MOLST or EMS PACD must be completed for all individuals on a standard form approved by the Division of Public Health, and the form must be present.
6.4 If any question exists as to the identity of the individual identified on the Delaware MOLST or EMS PACD form, the EMS provider shall seek to identify the individual through another form of positive identification.
7.4.1 If in doubt as to the identification of the individual, the EMS provider shall initiate resuscitative efforts.
7.1 Revocation by a Patient
7.1.1 A MOLST or EMS PACD may be revoked at any time by: an individual with capacity by:
7.1.1.1 A written cancellation signed by the individual; or
7.1.1.2 An oral statement or gesture of any manner by the individual in the presence of two (2) witnesses, one of whom is a health care provider, requesting only palliative care or resuscitation; or
7.1.1.3 A new MOLST/PACD constitutes a revocation of a previously dated MOLST/PACD.
7.1.2 If the individual revokes a MOLST form or an EMS PACD orally, the EMS PACD notification devices do not need to be destroyed. EMS providers should thoroughly document the circumstances of the revocation. An oral revocation by an individual is only good for the single response or transport for which it was issued.
7.2 Revocation by an agent, guardian, or surrogate.
7.2.1 During an emergency, when the authorized decision maker is not the individual, this decision maker cannot revoke a MOLST order or an EMS PACD. Under no circumstances, can a person or entity, other than the individual, revoke a MOLST order or an EMS PACD during an emergency.
7.2.2 Because of the difficulty in identifying authorized decision makers in emergent situations, it is incumbent upon an authorized decision maker who has authority to revoke a MOLST order or an EMS PACD to do so prior to the emergency if they wish resuscitation for the individual.
16 Del.C. ??2513(b) makes willful concealment, destruction, falsification or forging of an advance directive, without the individual's or authorized decision maker's consent, a class C felony.
9.1 Nothing in these regulations shall affect the power of EMS providers to do the paramedic field termination of resuscitation protocol as approved by the Delaware Board of Medical Licensure and Discipline.
9.2 A life-sustaining procedure may not be withheld or withdrawn from a patient known to be pregnant, so long as it is probable that the fetus will develop to be viable outside the uterus with the continued application of a life-sustaining procedures. (16 Del.C. ??2503(i))
10.1 The Division of Public Health, in consultation with the Board of Medical Licensure and Discipline and the Delaware Fire Prevention Commission, shall develop and publish a protocol for EMS providers to comply with the requirements of this regulation.
10.2 The MOLST form will be available online, in order to maintain continuity throughout Delaware, please copy or print the MOLST form on purple or violet paper.
10.2.3 Faxed copies and photocopies are also valid MOLST forms.
10.2.4 Once this regulation has taken effect and the new MOLST forms are available online, health care providers and patients should no longer use the PACD form, but should use the MOLST form instead.
10.2.4.1 Although new PACD forms should not be created after the MOLST form becomes available, any PACD forms already completed with be honored.
11.1 The MOLST form does not expire, but it should be reviewed periodically whenever:
11.1.1 The person is transferred from one care setting or care level to another, or
11.1.2 There is a substantial change in the person???s health status, or
11.1.3 The person???s treatment preferences change.
11.2 To void the MOLST form, draw a line through ???Medical Orders??? and write ???VOID??? in large letters. Any changes require a new MOLST.
12.1 In addition to other immunity that may be provided for in law, 16 Del.C. ??2510 provides specific immunity in cases involving the provision, withdrawal, or withholding of care which may be life sustaining in nature.
12.1.1 EMS providers are not subject to criminal prosecution or civil liability or deemed to have engaged in unprofessional conduct as determined by the appropriate licensing, registering, or certifying authority as a result of withholding or withdrawing any healthcare under authorization obtained in accordance with 16 Del.C. Ch. 25.
13.1 The Division of Public Health shall provide appropriate information, education and training on the EMS PACD Program to health care providers.
13.2 The Division of Public Health shall monitor the use of MOLST or EMS PACDs as presented to EMS providers.
13.3 The Division shall take such measures as necessary to assure individual confidentiality.
Standardized EMS-Do Not Resuscitate (DNR) or MOLST or POLST (Physician Order for Life-Sustaining Treatment) orders validly executed and in compliance with the laws of that state shall be honored subject to the limitations in these regulations.
4304 Delaware Medical Orders for Scope of Treatment (DMOST)
These DMOST regulations implement 16 Del.C. Ch. 25A which authorizes the Division of Public Health/Office of Emergency Medical Services, in conjunction with the Board of Medical Licensure and Discipline, the Delaware EMS Oversight Council, the Delaware State Fire Prevention Commission, and other key groups within the State to develop and implement DMOST regulations and protocol. These regulations, protocol, and form standardize documentation so that Emergency Medical Service (EMS) personnel and all health-care providers have a readily recognizable form which sets forth a patient???s preferences regarding the provision of and the scope of treatment. The DMOST form allows EMS personnel and other health-care providers both to identify and to honor an individual???s wishes to the greatest extent possible and to grant individuals the dignity, humanity, and compassion they deserve.
In order for EMS personnel to honor an individual???s request related to end-of-life decisions, the EMS provider must have a medical order. The DMOST form serves both as the summary of the individual???s advance health-care planning decisions and as the medical order.
"Advance health-care directive (AHCD)??? means an advance health-care directive under 16 Del.C. Ch. 25, a durable power of attorney for health-care decisions, or any individual instruction or power of attorney for health care valid under Delaware law in the state where such document was executed or where the individual executing such document was a resident at the time that such document appointing an agent was executed. Said document must have been executed by the individual authorizing the appointed agent to make decisions about the individual's health care when such individual no longer has decision-making capacity.
???Decision-making capacity??? means a patient's ability to understand and appreciate the nature and consequences of a particular health-care decision, including the benefits and risks of that decision and alternatives to any proposed health care treatment, and to reach an informed health-care decision.
???Delaware Medical Orders for Scope of Treatment (DMOST)??? means a clinical process to facilitate communication between health-care professionals and a patient living with serious illness or frailty whose health-care practitioner would not be surprised if the patient died within the next year or, if the patient lacks decision-making capacity, the patient???s authorized representative. The process encourages shared, informed medical decision-making.The decisions are memorialized in a completed DMOST form, which contains portable medical orders that respect the patient???s goals for care with respect to the use of CPR and other life-sustaining treatments and medical interventions. The DMOST form is applicable across health-care settings, is reviewable, and can be voided.
???Department??? means the Department of Health and Social Services.
???DMOST form??? means the standardized document created by the Department that is identified as an Attachment to these regulations, which:
???Emergency-care provider??? means an emergency medical technician, paramedic, or first responder authorized under 16 Del.C. Ch 97.
???Health-care institution??? means an institution, facility, or agency licensed, certified or otherwise authorized or permitted by law to provide health care in the ordinary course of business.
???Health-care practitioner??? means a physician or an individual licensed and authorized to write medical orders pursuant to 24 Del.C. Ch. 17 and Ch. 19 who is providing care for the patient or overseeing the health care provided to the patient and has completed all training required by the Department for individuals participating in the completion of a DMOST form. Over time, a patient???s health-care practitioner may change.
???Health-care provider??? means an individual licensed, certified, or otherwise authorized or permitted by law to provide health care in the ordinary course of business or practice of a profession. A health-care practitioner is also a health-care provider.
???Life-sustaining treatment??? includes any medical intervention, including procedures, administration of medication, or use of a medical device, that maintains life by sustaining, restoring, or supplanting a vital function. It does not include care provided for the purpose of keeping a patient comfortable.
???Patient??? means an individual who is under the care of the health-care practitioner or health-care provider.
???Patient???s authorized representative??? or ???authorized representative??? means the individual signing a DMOST form on behalf of a patient without decision-making capacity, who has the highest priority to act for the patient under law, and who has the authority to make decisions with respect to the patient???s health-care preferences being made on the DMOST form. The health-care practitioner shall determine the individual who is the patient???s authorized representative by referencing the documentation giving such individual the required authority under law. Based on the documentation provided by such individual as evidence of his or her authority, the patient???s authorized representative could be an individual designated by a patient under an advance health-care directive, an agent under a medical durable power of attorney for health-care decisions, a guardian of the person appointed pursuant to 12 Del.C. Ch. 39 or Ch. 39A, in accordance with the authority granted by the appointing court, a surrogate appointed under 16 Del.C. Ch. 25, or an individual who is otherwise authorized under applicable law to make the health-care decisions being made by execution of the DMOST form on the patient???s behalf, if the patient lacks decision-making capacity.
???Scope of treatment??? means those medical interventions, procedures, medications, and treatments that a patient, in consultation with a health-care practitioner, has determined are appropriate, necessary, and desired by and for the patient and will always include the provision of comfort measures. A patient may decline life-sustaining treatment.
???Serious illness or frailty??? means a condition for which a health-care practitioner would not be surprised if a patient died within the next year.
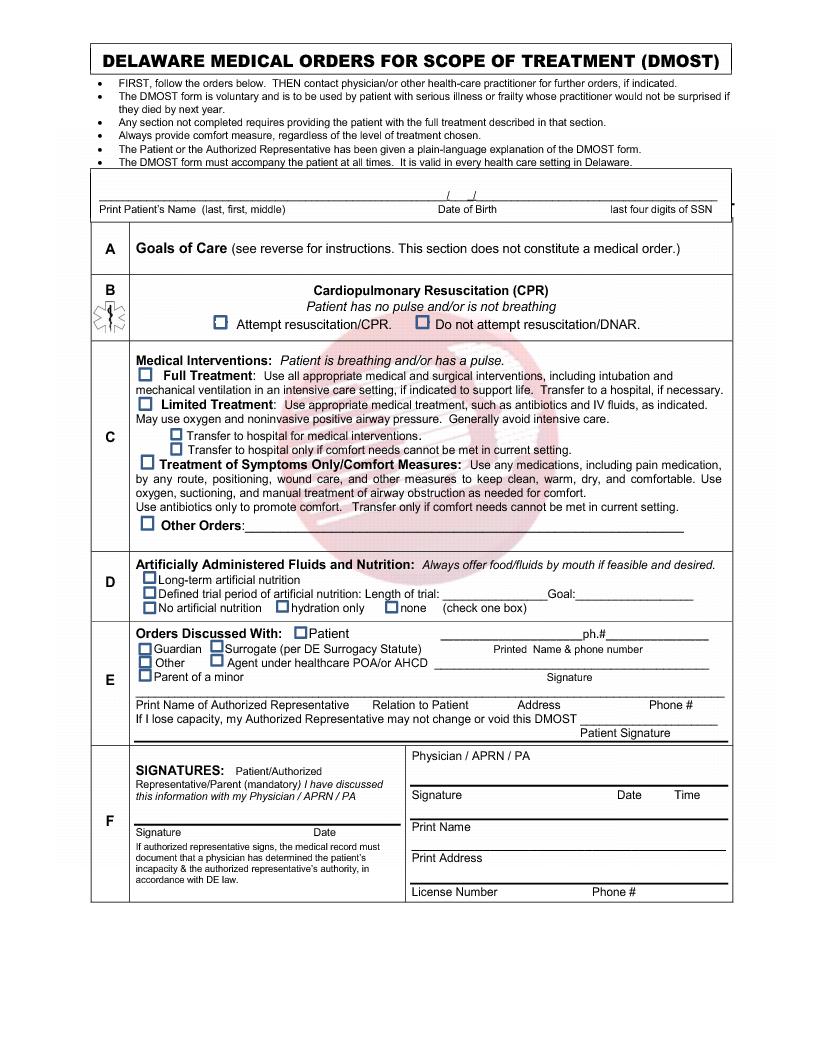
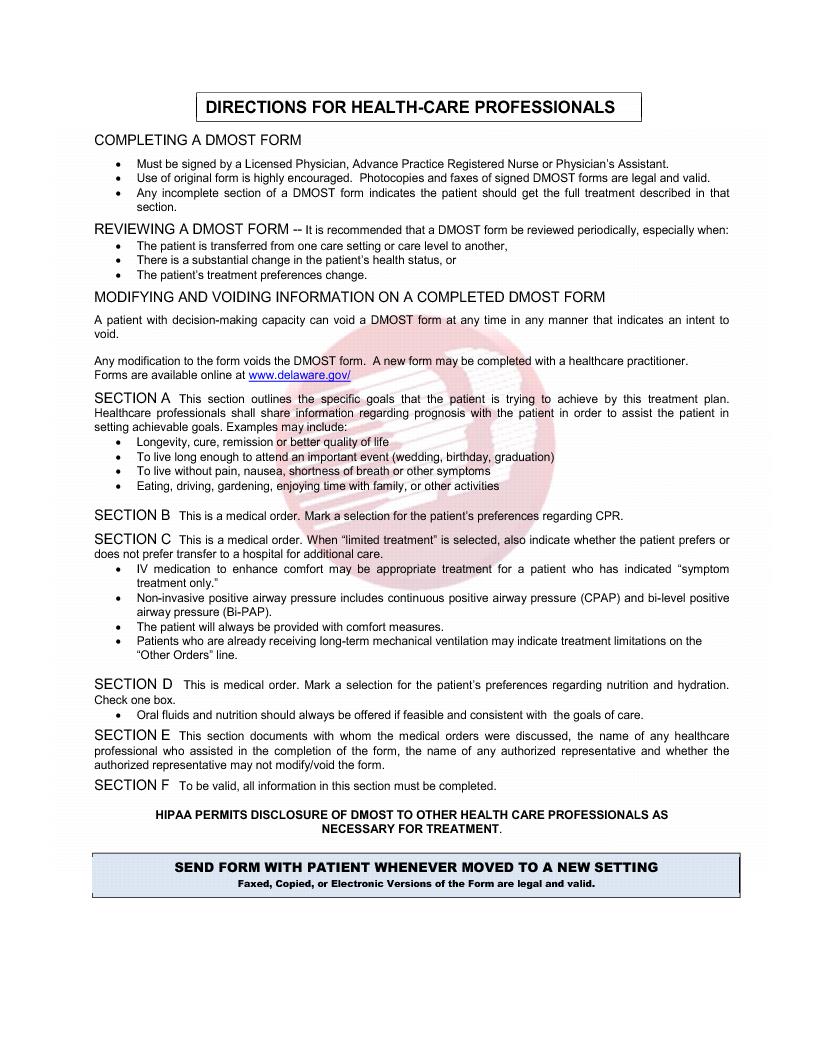
2.1 The DMOST Form, including instructions for completion and plain language explanation, is published in these regulations. The DHSS documents in these regulations may not be altered.
2.1.1 The patient???s identification block has the patient???s name (last, first, middle), date of birth, and last four digits of the patient???s social security number.
2.1.2 The Scope of Treatment sections are Blocks A to E.
2.1.2.1 Section A contains the goals of care. This section is for the patient to draft a goal statement relative to their current treatment plan. This section does not constitute a medical order.
2.1.2.2 Section B contains Cardiopulmonary Resuscitation decision (when the patient has no pulse and/or is not breathing). This section constitutes a medical order.
2.1.2.3 Section C contains Medical Interventions (when patient is breathing and/or has a pulse). This section has four categories to be answered. This section constitutes a medical order.
2.1.2.3.1 Treatment of symptoms only/Comfort Measures Only. Use any medications, including pain medication, by any route, positioning, wound care, and other measures to keep clean, warm, dry, and comfortable. Use of oxygen, oral suctioning and manual treatment of airway obstruction as needed for comfort. Use antibiotics only to promote comfort. Transfer if comfort needs cannot be met in current location.
2.1.2.3.2 Limited Treatment. Includes care described above, and use appropriate medical treatment such as antibiotics and IV fluids, and cardiac monitoring as indicated. Do not use intubation or mechanical ventilations. May use non-invasive airway support that does not require the introduction of instruments into the body [e.g. CPAP, BIPAP] however if clearing the airway with manual techniques is unsuccessful, direct laryngoscopy and the use of Magill Forceps may be used. Generally avoid intensive care and transfer to hospital if ordered for medical interventions or if ordered because comfort needs cannot be met in current location.
2.1.2.3.3 Full Treatment. Includes care described above, and use all appropriate medical and surgical interventions, including intubation, advanced airway interventions, mechanical ventilation, and cardioversion, in an intensive care setting if indicated to support life. Transfer to hospital, if indicated, including intensive care.
2.1.2.3.4 Other orders. Provide the care stated.
2.1.2.4 Section D contains the blocks to determine the desire for the artificially administered fluids and nutrition.
2.1.2.5 Section E contains information as to whom the DMOST form was discussed with and it contains a signature block for the patient to authorize an authorized representative the ability to void the DMOST form and execute a new DMOST form that changes the treatment choices if the patient loses decision-making capacity.
2.1.3 The Signature blocks. Section F contains the signature areas for the patient/authorized representative/parent and the health-care practitioner. To be valid the form must have all required signatures in this block.
3.1 A DMOST form shall be deemed to be completed and therefore valid for the purposes of this chapter if it:
3.1.1 Contains information indicating the patient???s health-care preferences;
3.1.2 Has been voluntarily signed by the patient or by another individual subscribing the patient???s name in the patient???s presence and at the patient???s express direction, or, if the patient does not have decision-making capacity, by the patient???s authorized representative;
3.1.3 Contains a statement that the DMOST form is being signed after discussion with the patient, or if the patient lacks decision-making capacity, the patient???s authorized representative;
3.1.4 Includes the signature of the patient???s health-care practitioner and the date and time of the health-care practitioner???s signature;
3.1.5 If the DMOST form is not signed by the heath-care practitioner in the presence of the patient, the DMOST form will also be signed by the health-care provider in whose presence the patient or, if the patient does not have decision-making capacity, the patient???s authorized representative signed the DMOST form;
3.1.6 The DMOST form shall include a statement that the patient or, if the patient does not have decision-making capacity, the patient???s authorized representative, has been provided with the plain language statement explaining the DMOST form, and the consequences of executing the DMOST form, including whether or not the DMOST form may be changed if the patient lacks decision-making capacity.
4.1 Completing a DMOST form is always voluntary and cannot be required for any reason.
4.2 A DMOST form can only be used by a patient who is living with a serious illness or frailty whose health-care practitioner would not be surprised if the patient died within the next year.
4.3 The health-care practitioner must discuss the DMOST form directly with the patient, or if the patient lacks decision-making, the patient???s authorized representative, prior to completion.
4.4 A DMOST form must be signed by a health-care practitioner.
4.5 Only the DMOST form in these regulations, which contains a watermark, can be recognized as a DMOST form. Copies of signed DMOST forms are legal and valid to the same extent as the original.
4.6 If any section of a DMOST form is incomplete, the full treatment described in that section shall be administered to the patient.
4.7 The patient may have decision-making capacity but be unable to communicate by speaking or writing. In such situations:
4.7.1 The patient can make his or her health-care treatment decisions known through any method by which the patient usually communicates so long as the person interpreting the communication understands the method by which the patient is communicating and the substance of the communication; and
4.7.2 The communication and how it occurred must be documented in the patient???s medical record; and
4.7.3 If a patient cannot physically sign a DMOST form but has communicated that they want to sign the DMOST form, someone other than the patient can sign the DMOST form on behalf of the patient.
4.8 Delaware law presumes an adult has decision-making capacity unless a physician determines the patient does not.
4.9 If a physician determines a patient does not have decision-making capacity, this must be documented in the patient???s medical record. If an adult patient does not have decision-making capacity, an authorized representative may sign a DMOST form on behalf of the patient if the authorized representative has legal authority to do so.
4.9.1 The health-care practitioner shall determine if there is an individual who is the patient???s authorized representative. This is determined by referencing the documentation giving such individual the required authority under law. The documentation should establish both that the authorized representative is the person named in this role and that the authorized representative has the authority to sign the DMOST form on behalf of the patient.
4.9.2 The hierarchy under Delaware Law to act as the authorized-representative for a person without decision-making capacity is as follows:
4.9.2.1 The court-appointed Guardian, only with the appropriate authority;
4.9.2.2 The patient???s most recently appointed Agent in an Advance Health Care Directive or Health Care Power of Attorney, only with the appropriate authority;
4.9.2.3 If the there is no Guardian or Agent or if the designated Guardian or Agent is unavailable, or if the patient revoked an Advance Health Care Directive pursuant to 16 Del.C. ??2504, the Surrogate Statute applies and will allow either the individual named by the patient prior to losing decision-making capacity or if none, the individual recognized by the Surrogate Statute, 16 Del.C. ??2507, to act.
4.10 If the patient is under age 18, and therefore has no decision-making capacity, the hierarchy under Delaware law to act as the authorized representative for such minor patient is as follows, in descending order:
4.10.1 In the absence of any legal activity to the contrary, biological parents and court-appointed guardians;
4.10.2 The Division of Family Services (DFS) if it holds parental rights;
4.10.3 The DFS if it holds legal custody based on dependency or neglect and after reasonable efforts to contact and gain consent from the biological parents. If DFS takes custody, its authority is superior to that of any court-appointed guardian.
4.10.4 A caregiver acting under an Affidavit of Relative Caregiver under 13 Del.C. ????707, 708.
5.1 Any changes or alterations to the information on the completed DMOST form voids the form.
5.2 The content of a completed DMOST form can only be modified by voiding the current DMOST form and completing a new DMOST form.
5.3 A patient with decision-making capacity, may, at any time, void his or her completed DMOST form or otherwise request alternative treatment to the treatment that was ordered on the DMOST form in any manner that indicates the patient???s intent to void the DMOST form.
5.4 If a patient does not have decision-making capacity, an authorized representative may void and/or request a new DMOST form, based on the known wishes of the person, or if unknown, the person???s best interest, if the authorized representative has the legal authority to do so and is permitted to do so on the existing DMOST form completed by the patient.
Nothing in these regulations shall affect the authority of EMS providers to do the paramedic field termination of resuscitation protocol as approved by the Delaware Board of Medical Licensure and Discipline.
7.1 The Division of Public Health, in consultation with the Board of Medical Licensure and Discipline and the Delaware Fire Prevention Commission, shall develop and publish a protocol for EMS providers to comply with the requirements of this regulation.
7.2 Copies of a valid DMOST form are valid to the same extent as the original.
8.1 In the event of a disagreement between the patient???s authorized representative and the patient???s health-care practitioner concerning the patient's decision-making capacity or the appropriate interpretation and application of the terms of a completed DMOST form regarding the patient's course of treatment, the parties:
8.1.1 May seek to resolve the disagreement by means of procedures and practices established by the health-care institution, including, but not limited to, consultation with an institutional ethics committee, or with an individual designated by the health-care institution for this purpose; or
8.1.2 May seek resolution by a court of competent jurisdiction.
8.2 A health-care provider involved in the patient's care or an administrator of a health-care institution may seek to resolve a disagreement concerning the appropriate interpretation and application of the terms of a completed DMOST form to the patient's course of treatment in the same manner as set forth in 8.1.
8.3 In the event of conflicting directives, the patient???s scope of treatment shall be governed by the latest directive available.
8.3.1 If the treatment directives of a later Advance Health Care Directive conflict with the patient's directives on a DMOST form, a health-care practitioner shall be informed so that the DMOST form can be modified or voided in order to reflect that patient???s later directive.
8.3.2 If there is a conflict between the patient's expressed oral or written directives, the DMOST form, or the decisions of the patient???s authorized representative, the patient's last expressed oral or written directives shall be followed and, if necessary, a new DMOST form shall be prepared and executed to reflect those directives.
8.4 Any individual or entity may petition the Court of Chancery for appointment of a guardian of the person of a patient if that individual or entity has good reason to believe that the withdrawal or withholding of health care in a particular case:
8.4.1 Is contrary to the most recent expressed wishes of a patient;
8.4.2 Is predicated on an incorrect assessment of the patient???s decision-making capacity;
8.4.3 Is being proposed pursuant to a DMOST form that has been falsified, forged, or coerced;
8.4.4 Is being considered without knowledge of a voided completed DMOST form which has been unlawfully concealed, destroyed, altered, or cancelled; or
8.4.5 Is based on a patient???s status either as an individual with a pre-existing long-term mental or physical disability, or as an individual who is economically disadvantaged.
8.5 A health-care institution, health-care practitioner, or health-care provider acting in good faith and in accordance with generally accepted health-care standards applicable to the health-care institution, health-care practitioner, or health-care provider is not subject to civil or criminal liability or to discipline for unprofessional conduct for:
8.5.1 Complying with a DMOST form signed by a health-care practitioner apparently having authority to make a DMOST for a patient, including a decision to withhold or withdraw health care;
8.5.2 Declining to comply with a DMOST form based on a belief that the health-care practitioner then lacked authority to sign a DMOST;
8.5.3 Complying with a DMOST form and assuming that the DMOST form was valid when made and has not been modified or voided;
8.5.4 Providing life-sustaining treatment in an emergency situation when the existence of a DMOST form is unknown; or
8.5.5 Declining to comply with a DMOST form because the DMOST form is contrary to the conscience or good faith medical judgment of the health-care practitioner or the written policies of the health-care institution.
9.1 The Division of Public Health shall provide appropriate information, education and training on the DMOST Program to EMS personnel.
9.2 The Division of Public Health shall monitor the use of DMOST forms presented to EMS providers.
9.3 The Division of Public Health shall take such measures as necessary to assure individual confidentiality.
10.1 A DMOST Form transfers with a patient and the medical orders indicated on a DMOST form are valid in every health-care setting in Delaware. Copies of a valid DMOST form are valid to the same extent as the original.
10.2 A document executed in another state, which meets the requirements of this regulation for a DMOST form, the requirements of the state where such document was executed, or the state where the patient was a resident at the time the document was executed, shall be deemed to be valid for the purposes of 16 Del.C. Ch. 25A to the same extent as a DMOST form valid under that chapter.
DMOST is a process for documenting treatment choices.The DMOST form is voluntary. It is a portable, standardized Medical Order that will be recognized and followed by Delaware health care providers.
The DMOST conversation is an opportunity to understand the likely course of your health and medical condition, so that you may make informed choices that are appropriate and reflect what you want. If you choose, you may invite loved ones to join this conversation.
Q. What is DMOST?
A. The Delaware Medical Orders for Scope of Treatment (DMOST) form is a portable medical order form. It allows you to make choices about life-sustaining treatments, including among other treatments, CPR (resuscitation) and artificial nutrition.You may request full treatment, limited treatment, or comfort care only.
Q. Who is it for?
A. A DMOST form can be used by a person with a serious illness or frailty, whose health-care practitioner would not be surprised if they died within the next year.
Q. When should it be discussed and signed? Who signs it?
A. A DMOST form is completed after a conversation you have with a health care practitioner. It is signed by you and a physician (MD or DO), an advanced practice registered nurse (APRN), or a physician assistant (PA). The physician/APRN/PA signature makes the choices into portable medical orders.
Q. Who is required to follow the wishes documented on the DMOST form?
A. These orders will be followed by health care providers in any setting (ambulance, long-term care facility, emergency room, hospital, hospice, home, assisted living facility, etc.). It travels with you and is honored when you move to a new setting.
Q. Can someone else make DMOST decisions for me?
A. You make health-care decisions for yourself as long as you have decision-making capacity. You have the right to change your authorized representative at any time while you have decision-making capacity.
If a physician determines that a person lacks decision-making capacity, an authorized representative can sign a DMOST form on behalf of that person. A DMOST form does not change the decision-maker designated by an Advance Health Care Directive, a Health Care Power of Attorney document, a guardian of person appointed by a Court, or Delaware law on health care surrogates.
If you have capacity and complete a DMOST form, you can sign on the form saying that if you lose capacity, your authorized representative cannot void the form you signed.
Q. What if I change my mind?
A. If your condition or your choices change, you or your authorized representative should void (cancel) your DMOST form and request a new DMOST be completed with your new choices. You can void a DMOST form if you change your mind but do not want to create a new one. You may not make any changes to the content of the DMOST form. If you want to change your DMOST form you must void your previous form and complete a new one with your health-care practitioner. If your DMOST form does not agree with your advance directive, the most recent document will be followed.
Q. Must I do this?
A. The DMOST form is always voluntary and can be voided at any time. A Health care organization is prohibited from requiring you to complete a DMOST form for any reason, including as part of a person???s admission to a health care facility.
It is important to understand that this form contains medical orders. It will be followed by health care providers. For example, if you choose ???Do Not Attempt Resuscitation???, and your heart stops, no attempt will be made to restart your heart. If you choose ???Intubate/Use Artificial ventilation???, then you may be placed on a breathing machine with a tube in your throat and transferred to an intensive care setting in a hospital.
Q. What will happen to my choices if I travel out of state?
A. Many states, including all the states in our region, currently use a form similar to the DMOST form. Forms from those states which are valid under the Delaware Law will be honored in Delaware. DMOST forms will be honored in other states which have reciprocity.







