DEPARTMENT OF HEALTH AND SOCIAL SERVICES
Division of Medicaid and Medical Assistance
PROPOSED
PUBLIC NOTICE
Third Party Liability
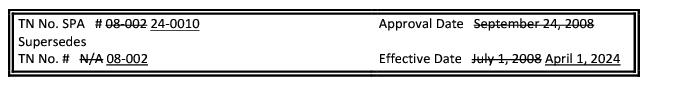
In compliance with the State's Administrative Procedures Act (APA - Title 29, Chapter 101 of the Delaware Code) and under the authority of 31 Del.C. §512, Delaware Health and Social Services ("Department") / Division of Medicaid and Medical Assistance (DHSS/DMMA) is proposing to amend Title XIX Medicaid State Plan Attachment 4.11-A - Attachment 7.7.C Supplement to Attachment 4.22, specifically, to comply with the Consolidated Appropriations Act of 2022 and Senate Bill 220 of the 152nd Delaware General Assembly.
Any person who wishes to make written suggestions, compilations of data, testimony, briefs, or other written materials concerning the proposed new regulations must submit same to, Planning and Policy Unit, Division of Medicaid and Medical Assistance, 1901 North DuPont Highway, P.O. Box 906, New Castle, Delaware 19720-0906, by email to DHSS_DMMA_Publiccomment@Delaware.gov, or by fax to 302-255-4413 by 4:30 p.m. on May 31, 2024. Please identify in the subject line: Third Party Liability
The action concerning the determination of whether to adopt the proposed regulation will be based upon the results of Department and Division staff analysis and the consideration of the comments and written materials filed by other interested persons.
SUMMARY OF PROPOSAL
The purpose of this notice is to advise the public that Delaware Health and Social Services (DHSS)/Division of Medicaid and Medical Assistance (DMMA) is proposing to amend Title XIX Medicaid State Plan regarding Third Party Liability.
Statutory Authority
Background
Medicaid is generally the "payer of last resort," meaning that Medicaid only pays claims for covered items and services if there are no other liable third-party payers for the same items and services. When Medicaid beneficiaries have one or more additional sources of coverage for health care services, third-party liability (TPL) rules govern the legal obligation of such third parties. Section 1902(a)(25)(A) of the Social Security Act defines third-party payers as health insurers, managed care organizations, and group health plans, among others.
The federal Consolidated Appropriations Act of 2022 (CAA 2022), enacted March 15, 2022, increased state flexibility with respect to TPL. Section 202 of the CAA, 2022 amended section 1902(a)(25)(I) of the Act to require a state plan for medical assistance to provide assurances satisfactory to the Secretary that the state has state laws in place that bar responsible third-party payers (other than Medicare plans) from refusing payment for an item or service solely on the basis that such item or service did not receive prior authorization under the third-party payer's rules. Specifically, if the responsible third party requires prior authorization for an item or service furnished to a Medicaid-eligible individual, the responsible third party must accept the authorization provided by the state that the item or service is covered under the state plan (or waiver of such plan) for such individual, as if such authorization was made by the third party for such item or service. Authorization by the state means that the item or service an individual received (and for which third-party reimbursement is being sought) is a covered service or item under the Medicaid state plan (or waiver of such plan) for that individual.
On March 28, 2024, Senate Bill 220 of the 152nd General Assembly, An Act to Amend Title 18 Relating to Health Insurance for Children And Persons On Medicaid received enough votes to pass the both the Senate and House, moving the bill forward for Governor's signature. This bill updates the provisions of Title 18, § 4003 to make them consistent with federal law contained in the Consolidated Appropriations Act of 2022.
Summary of Proposal
Purpose
The purpose of this proposed regulation is to comply with current law revise the Medicaid State Plan to align with the CAA, 2022 requirements and SB 220.
Summary of Proposed Changes
Effective April 1, 2024, the DHSS/DMMA proposes to amend Title XIX Medicaid State Plan regarding Third Party Liability, specifically, to comply with CAA, 2022 and SB 220.
Public Notice
In accordance with the federal public notice requirements established in Section 1902(a)(13)(A) of the Social Security Act and 42 CFR 440.386 and the state public notice requirements of Title 29, Chapter 101 of the Delaware Code, DHSS/DMMA gives public notice and provides an open comment period for 30 days to allow all stakeholders an opportunity to provide input on the proposed regulation. Comments must be received by 4:30 p.m. on May 31, 2024.
Centers for Medicare and Medicaid Services Review and Approval
The provisions of this state plan amendment (SPA) are subject to approval by the Centers for Medicare and Medicaid Services (CMS). The draft SPA page(s) may undergo further revisions before and after submittal to CMS based upon public comment and/or CMS feedback. The final version may be subject to significant change.
Provider Manuals and Communications Update
Also, there may be additional provider manuals that may require updates as a result of these changes. The applicable Delaware Medical Assistance Program (DMAP) Provider Policy Specific Manuals and/or Delaware Medical Assistance Portal will be updated. Manual updates, revised pages or additions to the provider manual are issued, as required, for new policy, policy clarification, and/or revisions to the DMAP program. Provider billing guidelines or instructions to incorporate any new requirement may also be issued. A newsletter system is utilized to distribute new or revised manual material and provide other pertinent information regarding DMAP updates. DMAP updates are available on the Delaware Medical Assistance Portal website: https://medicaid.dhss.delaware.gov/provider
Fiscal Impact
This change will result in a cost avoidance therefore there is no fiscal impact.
Supplement to Attachment 4.2.2
STATE PLAN UNDER TITLE XIX OF THE SOCIAL SECURITY ACT
STATE/TERRITORY: DELAWARE
|
1902(A)(25)(I)
|
The State has in effect laws that require third parties to comply with the provisions, including those which require third parties to provide the State with coverage, eligibility and claims data, of 1902(A)(25)(I) of the Social Security Act.
|
|
|
The Medicaid agency ensures that laws are in effect that bar liable third-party payers from refusing payment for an item or service solely on the basis that such item or service did not receive prior authorization under the third-party payer's rules. These laws comply with the provisions of section 202 of the Consolidated Appropriations Act, 2022.
|