DEPARTMENT OF HEALTH AND SOCIAL SERVICES
Division of Medicaid and Medical Assistance
FINAL
ORDER
Non-Emergency Medical Transportation (NEMT)
NATURE OF THE PROCEEDINGS:
Delaware Health and Social Services (Department) / Division of Medicaid and Medical Assistance (DMMA) initiated proceedings to amend Title XIX Medicaid State Plan regarding transportation, specifically, to establish coverage and reimbursement methodologies for non-emergency medical transportation (NEMT) services. The Department's proceedings to amend its regulations were initiated pursuant to 29 Del. C. § 10114 and its authority as prescribed by 31 Del. C. § 512.
The Department published its notice of proposed regulation changes pursuant to 29 Del. C. § 10115 in the January 2020 Delaware Register of Regulations, requiring written materials and suggestions from the public concerning the proposed regulations to be produced by January 31, 2020 at which time the Department would receive information, factual evidence and public comment to the said proposed changes to the regulations.
SUMMARY OF PROPOSAL
Effective for services provided on and after February 11, 2021 Delaware Health and Social Services/Division of Medicaid and Medical Assistance (Department/DMMA) proposes to amend Attachment 3.1-A Page 9a and Attachment 4.19-B Page 3 of Title XIX Medicaid State Plan regarding transportation, specifically, to establish coverage and reimbursement methodologies for non-emergency medical transportation (NEMT) services.
Background
The Medicaid non-emergency medical transportation (NEMT) benefit is authorized under the Social Security Act under section 1902(a)(70) and 42 CFR § 440.170. It ensures necessary transportation to and from providers and includes coverage for transportation and related travel expenses necessary to secure medical examinations and treatment.
Statutory Authority
Purpose
The purpose of this final regulation is to establish coverage and reimbursement methodologies for lodging related non-emergency medical transportation (NEMT) services for all Medicaid eligible individuals.
Public Notice
In accordance with the federal public notice requirements established at Section 1902(a)(13)(A) of the Social Security Act and 42 CFR 447.205, and the state public notice requirements of Title 29, Chapter 101 of the Delaware Code, the Department/DMMA gives public notice and provides an open comment period for thirty (30) days to allow all stakeholders an opportunity to provide input on the proposed regulation. Comments were to have been received by 4:30 p.m. on January 31, 2020.
Centers for Medicare and Medicaid Services Review and Approval
The provisions of this state plan amendment (SPA) are subject to approval by the Centers for Medicare and Medicaid Services (CMS). The draft SPA page(s) may undergo further revisions before and after submittal to CMS based upon public comment and/or CMS feedback. The final version may be subject to significant change.
Provider Manuals and Communications Update
Also, there may be additional provider manuals that may require updates as a result of these changes. The applicable Delaware Medical Assistance Program (DMAP) Provider Policy Specific Manuals and/or Delaware Medical Assistance Portal will be updated. Manual updates, revised pages, or additions to the provider manual are issued, as required, for new policy, policy clarification, and/or revisions to the DMAP program. Provider billing guidelines or instructions to incorporate any new requirement may also be issued. A newsletter system is utilized to distribute new or revised manual material and to provide any other pertinent information regarding DMAP updates. DMAP updates are available on the Delaware Medical Assistance Portal website: https://medicaid.dhss.delaware.gov/provider.
Fiscal Impact Statement
The anticipated fiscal impact is below: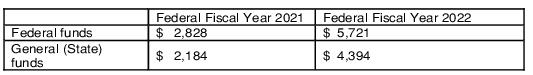
Summary of Comments Received with Agency Response and Explanation of Changes
The following summarized comments were received:
Comment: One commenter questioned what entity would be making the medical necessity evaluation or how this would be documented.
Agency Response: DMMA will take this into account in developing medical necessity and prior authorizations processes.
Comment: One commenter recommended that the regulation be revised to allow for the difficulty faced by single parents/guardians, particularly those with multiple children. Instead of “one authorized escort,” the regulation should allow for an exception for parents/guardians who cannot support the child in need of care without an additional sibling(s) in attendance.
Agency Response: 42 CFR 440.170(a)(3)(iii) allows states to include travel expenses for an attendant to accompany a beneficiary, if necessary. It does not allow for the state to cover travel expenses for additional members of the beneficiary’s family. The policy does not preclude additional members of the family from attending; however, it limits authorization of and payment for lodging or meals and lodging related to travel to the beneficiary and one authorized escort.
Comment: Two commenters endorsed the proposed regulation.
Agency Response: DMMA appreciates the endorsement.
DMMA is pleased to provide the opportunity to receive public comments and greatly appreciates the thoughtful input given by:
FINDINGS OF FACT:
The Department finds that the proposed changes as set forth in the January 2020 Register of Regulations should be adopted.
THEREFORE, IT IS ORDERED, that the proposed regulation to amend Title XIX Medicaid State Plan regarding transportation, specifically, to establish coverage and reimbursement methodologies for non-emergency medical transportation (NEMT) services, is adopted and shall be final effective February 11, 2021.
1/13/2021
Date of Signature
Molly K. Magarik, Secretary, DHSS
Revision: CMS Attachment 3.1-A
Page 9a
STATE PLAN UNDER TITLE XIX OF THE SOCIAL SECURITY ACT
STATE/TERRITORY: DELAWARE
SECTION 3 – SERVICES: GENERAL PROVISIONS
3.1 Amount, Duration, and Scope of Services
Medicaid is provided in accordance with the requirements of section 1902(a), 1902(e), 1903(i), 1905(a), 1905(p),
1905(r), 1905(s), 1906, 1915, 1916, 1920, 1925, 1929 and 1933 of the Act; section 245A(h) of the Immigration and
Nationality Act; and 42 CFR Parts 431, 440, 441, 442 and 483.
A. Categorically Needy
24. Any other medical care, and other type of remedial care recognized under State law, specified by law
Secretary (in accordance with section 1905(a)(28) of the Social Security Act and 42 CFR 440.170).
a. Transportation (provided in accordance with 42 CFR 440.170 as an optional medical service) excluding
“school-based” transportation.
☒ Provided without a broker as an optional medical [services service]: Payment may be made for the following
non-emergency medical transportation services when:
i. Lodging Service – Transportation-related services authorized by the single state agency to provide
overnight lodging for eligible recipients and, with prior authorization, one authorized escort.
Provider Requirements:
a. Lodging service providers must enroll with the state Medicaid program directly into the Delaware
Medicaid claims processing system; and
b. Providers must submit for reimbursement directly into the Delaware Medicaid claims
processing system.
ii. Lodging and Meals Service – Transportation-related services authorized by the single state agency to
provide overnight lodging, which includes meals (such as Ronald McDonald Houses), for eligible recipients
and, with prior authorization, one authorized escort.
Provider Requirements –
a. Lodging and Meals providers must enroll with the state Medicaid program; and
b. Providers must submit for reimbursement directly into the Delaware Medicaid claims processing
system.
c. Limitations – In the event that the member is admitted as inpatient, and provided meals via that
inpatient admission, meals for the member will not be covered.
(If state attests “Provided without a broker as an optional medical service” then insert supplemental information.)
Describe below how the transportation program operates including types of transportation and transportation
related services provided and any limitations. Describe emergency and non-emergency transportation services
separately. Include and interagency or cooperative agreements with other Agencies or programs.
☒ Non-emergency transportation is provided through a brokerage program as an optimal medial medical service
in accordance with 1902(a)(70) of the Social Security Act and 42 CFR 440.170(a)(4).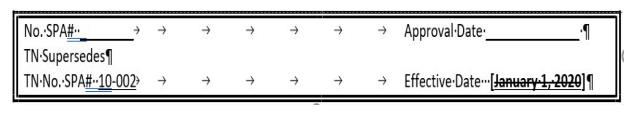
Attachment 4.19-B
Page 3a
STATE PLAN UNDER TITLE XIX OF THE SOCIAL SECURITY ACT
STATE/TERRITORY: DELAWARE
METHODS AND STANDARDS FOR ESTABLISHING PAYMENT RATES-
OTHER TYPES OF CARE
1. Emergency Transportation: Effective for dates of service on or after January 1, 2012, emergency
transportation is reimbursed as a percentage of the Medicare Fee Schedule for Delaware as follows:
2. Non-emergency Transportation without a broker: Effective for dates of service on or after January 1, [2020 2021],
non-emergency transportation services provided by transportation service providers enrolled with the state
Medicaid program who submit for reimbursement directly are reimbursed as follows:
both government and private providers of Lodging services. The agency’s Lodging fee schedule is
effective for services provided on and after January 1,[2020 2021]. The fee schedule and any annual/periodic
adjustments to the fee schedule are available on the DMAP website at:
http://www.dmap.state.de.us/downloads.
3. Non-emergency Transportation with a broker: The broker is reimbursed a monthly capitated rate for
each Medicaid client residing in the State.
Other Types of Care, Physician, Podiatry and Independent Radiology Services.
Except as otherwise noted in the Plan, State-developed fee schedule rates are the same for both governmental
and private individual practitioners. The fee schedule and any annual/periodic adjustments to the fee schedule are
published and found at: https://www.dmap.state.de.us/downloads/hcpcs.html.
Spectacle frames and lenses and contact lenses and are reimbursed based on Level II HCPCS procedure codes. The
agency's fee schedule rate for these procedure codes was set on July 1, 2002 and is available on the DMAP website.
provider's usual and customary charge or Delaware’s rate/cap, whichever is lower.
Where there is no universal rate/cap (i.e. providers are paid a provider-specific rate), Delaware Medicaid will
establish a rate or cap that is consistent with the reimbursement methodology defined in other sections of
Attachment 4.19-B for that specific service and pay the provider the lower of that rate/cap or their usual and
customary charge.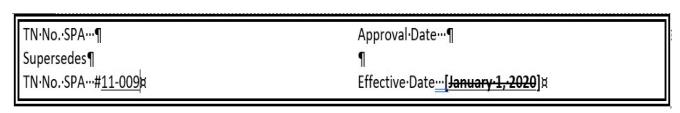
Attachment 4.19-B
Page 3b







