DEPARTMENT OF HEALTH AND SOCIAL SERVICES
Division of Medicaid and Medical Assistance
PROPOSED
PUBLIC NOTICE
Delaware Medicaid Modified Adjusted Gross Income (MAGI) Eligibility and Benefits State Plan Amendments
Citizenship and Immigration Status
In compliance with the State's Administrative Procedures Act (APA - Title 29, Chapter 101 of the Delaware Code) and under the authority of Title 31 of the Delaware Code, Chapter 5, Section 512 and with 42 CFR §447.205, Delaware Health and Social Services (DHSS) / Division of Medicaid and Medical Assistance (DMMA) is proposing to amend the Title XIX Medicaid State Plan to modify eligibility standards and processes to conform to the requirements under the Affordable Care Act, and to exercise available related state options. This SPA regulatory action deals with Citizenship and Immigration Status.
Any person who wishes to make written suggestions, compilations of data, testimony, briefs or other written materials concerning the proposed new regulations must submit same to Sharon L. Summers, Planning & Policy Development Unit, Division of Medicaid and Medical Assistance, 1901 North DuPont Highway, P.O. Box 906, New Castle, Delaware 19720-0906 or by fax to 302-255-4425 by October 31, 2013.
The action concerning the determination of whether to adopt the proposed regulation will be based upon the results of Department and Division staff analysis and the consideration of the comments and written materials filed by other interested persons.
SUMMARY OF PROPOSAL
The Division of Medicaid and Medical Assistance (DMMA) hereby affords the public notice of the filing of federally required state plan amendments (SPA) to modify eligibility standards and processes to conform to the requirements under the Affordable Care Act, and to exercise available related state options. This SPA regulatory action deals with Citizenship and Immigration Status.
Statutory Authority
Patient Protection and Affordable Care Act (Pub. L. No. 111-148 as amended by the Health Care and Education Reconciliation Act of 2010 (Pub. L. No. 111-152)), together known as the Affordable Care Act
Background
The Affordable Care Act (ACA) was signed into law on March 23, 2010. Under the ACA, health reform will make health care more affordable, guarantee choices when purchasing health insurance, expands Medicaid coverage to millions of low-income Americans and makes numerous improvements to both Medicaid and the Children’s Health Insurance Program (CHIP).
The Affordable Care Act (ACA) includes many provisions designed to expand and streamline Medicaid eligibility. The ACA offers the option to extend coverage to non-disabled, non-elderly citizens with income under 133 percent of the Federal Poverty Level (FPL); adopts new methodologies for determining and renewing eligibility; and requires establishment of a streamlined process to allow state Medicaid programs to coordinate seamlessly with other insurance affordability programs and affordable health insurance exchanges. These provisions are intended to change the Medicaid eligibility determination and renewal processes for most Medicaid applicants and beneficiaries from one based on a welfare model to one that utilizes information technology to provide the insurance coverage option that fits each individual’s current circumstances and needs.
State Plan Amendments
In preparation for implementation of the Medicaid and CHIP changes related to the Affordable Care Act, states will be submitting a number of State Plan Amendments (SPAs). In particular, SPAs are needed to implement the MAGI-based eligibility levels and income counting methodologies for Medicaid and CHIP, to elect a state’s single streamlined application format, and to indicate the design of their Medicaid alternative benefit plans (ABPs) for the new adult group in 2014. The vehicle for submitting these 2014-related SPAs are a set of “fillable” preprint documents. The Centers for Medicare and Medicaid Services (CMS) has asked states to submit these plan amendments together in order to provide a more comprehensive picture of the state’s proposed eligibility framework.
Please note that provisions and conditions that are required of all states are pre-checked and do not require any entry by the state. Also, by agreeing to any assurance the state is agreeing to comply with these requirements and conditions. The state provides this affirmative assurance by checking the box where indicated.
Description of State Plan Amendments and Effective Date
The MAGI and CHIP Eligibility and Benefit SPAs identify the groups that Delaware will cover in the Delaware Medicaid program. There are mandatory and optional coverage groups. These SPAs also identify the income limits for each group, if any, and criteria that the state has the option of selecting. The effective date of the following SPAs is October 1, 2013.
Delaware Medicaid MAGI SPAs include:
1. MAGI-Based Eligibility Group
This SPA identifies the mandatory and optional coverage groups that Delaware will cover.
2. Eligibility Process
This SPA identifies the use of Delaware’s single, streamlined application and the methods by which an application is accepted. It also includes renewal processing.
3. MAGI Income Methodology
This SPA identifies certain MAGI options Delaware has chosen.
4. Single State Agency
This SPA identifies Delaware Health and Social Services (DHSS)/Division of Medicaid and Medical Assistance (DMMA) as the Medicaid agency.
5. Residency
This SPA identifies the state's residency requirements.
6. Citizenship and Immigration Status
This SPA identifies the immigrant statuses eligible for Medicaid services. It also provides for a 90 day reasonable opportunity period for individuals who declare they are citizens or qualified immigrants to provide documentation. During this reasonable opportunity period, Delaware Medicaid must approve benefits if otherwise eligible.
CHIP MAGI Eligibility SPAs include:
1. MAGI Eligibility & Methods
These SPAs identify the groups covered under Delaware’s Title XXI CHIP program (Delaware Healthy Children Program).
2. Title XXI Medicaid Expansion
This SPA identifies ACA expansion coverage for children age 6-18 years with income between 100% FPL up to 133% FPL.
3. Eligibility Process
This SPA identifies the use of Delaware’s single, streamlined application and the methods by which Delaware Medicaid can accept an application. It also includes renewal processing.
4. Non-Financial Eligibility
These SPAs identify the CHIP programs non-financial eligibility criteria such as state residency, citizenship and lawful presence, and verification/use of applicant social security number.
REMINDER: In 2014, the following groups will not have any changes in eligibility for Medicaid and will remain eligible for Medicaid and will qualify based on current income and resource standards used today:
Summary of Proposal
Note: The statute and regulation cited are the Social Security Act and the Code of Federal Regulations.
Citizenship and Immigration Status
1902(a)(46)(B); 1903(v)(2), (3) and (4)
Proposed 42 CFR 435.4; 435.406; 435.956,
78 FR 4594 (issued on January 22, 2013)
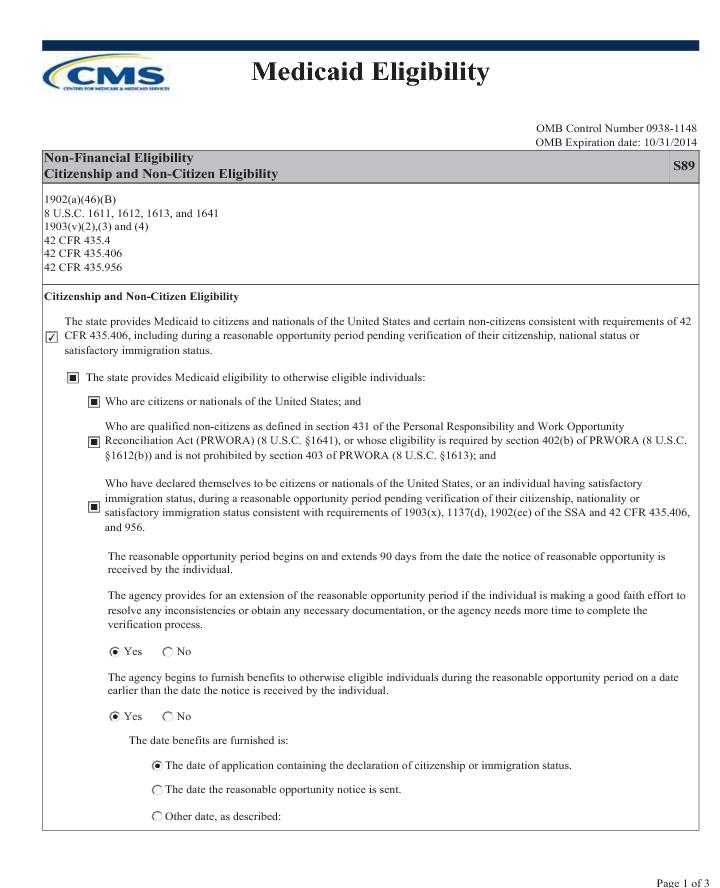
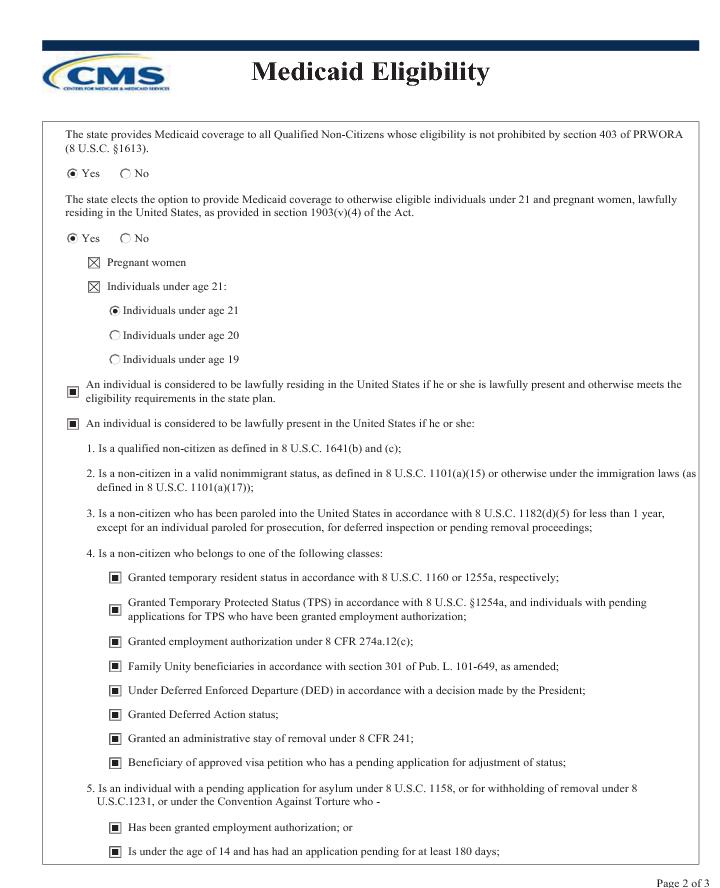
State plan page S89 describes the rules concerning Medicaid requirements related to U.S. citizenship and non-citizen eligibility.
Regulations at 42 CFR 435.406 require states to provide Medicaid to otherwise eligible individuals who are citizens or nationals of the United States, or qualified non-citizens as described in section 431 of the Personal Responsibility and Work Opportunity Reconciliation Act of 1996 (PRWORA) (8 U.S.C. 1641) and whose eligibility is not prohibited during the five year waiting period, required at 8 U.S.C. 1613 for certain qualified non-citizens.
Section 1137(d)(4) of the Social Security Act requires states to provide Medicaid to individuals having satisfactory immigration status during a reasonable period of time (known as a reasonable opportunity period) while their immigration status is being verified, if they are otherwise eligible for Medicaid.
Section 211 of the Children’s Health Insurance Program Reauthorization Act (CHIPRA) added the requirement to provide a reasonable opportunity period for an individual verifying their citizenship, if otherwise Medicaid eligible. Section 211 of CHIPRA amended section 1903(x) of the Act (requirement to provide documentary evidence of citizenship or nationality), and built upon existing regulation at §435.407(k) to require states to provide individuals who have declared themselves to be U. S. citizens, and who must have their citizenship or nationality status verified, the same reasonable opportunity to provide evidence of citizenship and to provide Medicaid coverage during this reasonable opportunity period, if the individual is otherwise Medicaid eligible, as is afforded to individuals who are verifying their immigration status.
The provisions of this state plan amendment are subject to approval by the Centers for Medicare and Medicaid Services (CMS).
Fiscal Impact Statement
|
Change to Federal Expenditures
|
State Fiscal Year
2014
|
State Fiscal Year
2015
|
|
Former CHIP Kids
|
$ 124,986
|
$ 254,855
|
|
ACA Expansion
|
$ 11,924,412
|
$ 26,689,670
|
|
Transitional
|
$ 187,657
|
$ 566,356
|
|
Former Foster Children
|
$ -
|
$ -
|
|
Total
|
$ 12,237,055
|
$ 27,510,882
|