DEPARTMENT OF HEALTH AND SOCIAL SERVICES
Division of Medicaid and Medical Assistance
FINAL
ORDER
Home Health Services
NATURE OF THE PROCEEDINGS:
Delaware Health and Social Services ("Department") / Division of Medicaid and Medical Assistance initiated proceedings to amend Title XIX Medicaid State Plan regarding Home Health Services, specifically, to add accreditation as an option to Medicare certification for Medicaid providers. The Department's proceedings to amend its regulations were initiated pursuant to 29 Delaware Code Section 10114 and its authority as prescribed by 31 Delaware Code Section 512.
The Department published its notice of proposed regulation changes pursuant to 29 Delaware Code Section 10115 in the September 2018 Delaware Register of Regulations, requiring written materials and suggestions from the public concerning the proposed regulations to be produced by October 1, 1018 at which time the Department would receive information, factual evidence and public comment to the said proposed changes to the regulations.
SUMMARY OF PROPOSAL
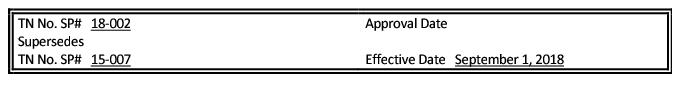
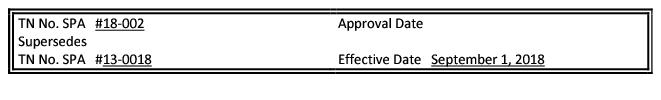
Effective for services provided on and after September 1, 2018 Delaware Health and Social Services/ Division of Medicaid and Medical Assistance proposes to amend Title XIX Medicaid State Plan page Attachment 4.19-B Page 6 and Attachment 3.1-A Page 3.1 Addendum regarding Home Health Services.
Background
Currently, to receive reimbursement, Delaware Medicaid providers must obtain Medicare certification.
Delaware Health and Social Services (DHHS)/Division of Medicaid and Medical Assistance (DMMA) has worked closely with the provider community to develop an alternative which provides flexibility and removes limitations.
Statutory Authority
Purpose
The purpose of this proposed regulation is to add accreditation as an option to Medicare certification for Medicaid providers.
Public Notice
In accordance with the federal public notice requirements established at Section 1902(a)(13)(A) of the Social Security Act and 42 CFR 447.205 and the state public notice requirements of Title 29, Chapter 101 of the Delaware Code, Delaware Health and Social Services (DHSS)/Division of Medicaid and Medical Assistance (DMMA) gives public notice and provides an open comment period for thirty (30) days to allow all stakeholders an opportunity to provide input on the proposed regulation. Comments were to have been received by 4:30 p.m. on October 1, 2018.
Centers for Medicare and Medicaid Services Review and Approval
The provisions of this state plan amendment (SPA) are subject to approval by the Centers for Medicare and Medicaid Services (CMS). The draft SPA page(s) may undergo further revisions before and after submittal to CMS based upon public comment and/or CMS feedback. The final version may be subject to significant change.
Provider Manuals and Communications Update
Also, there may be additional provider manuals that may require updates as a result of these changes. The applicable Delaware Medical Assistance Program (DMAP) Provider Policy Specific Manuals and/or Delaware Medical Assistance Portal will be updated. Manual updates, revised pages or additions to the provider manual are issued, as required, for new policy, policy clarification, and/or revisions to the DMAP program. Provider billing guidelines or instructions to incorporate any new requirement may also be issued. A newsletter system is utilized to distribute new or revised manual material and to provide any other pertinent information regarding DMAP updates. DMAP updates are available on the Delaware Medical Assistance Portal website: https://medicaid.dhss.delaware.gov/provider
Fiscal Impact Statement
There is no anticipated fiscal impact to the agency as a result of this proposed change in program policy.
Summary of Comments Received with Agency Response and Explanation of Changes
The initial Proposed Regulation for Home Health Services was published in the June 1, 2018 issue of the Delaware Register of Regulations (21 DE Reg. 951) with a comment period of June 1 - July 2. After consideration of public comments, the Proposed regulation was reprinted as Proposed in the September 1, 2018 issue of the Delaware Register of Regulations and there were no comments received as a result of that publication.
FINDINGS OF FACT:
The Department finds that the proposed changes as set forth in the September 2018 Register of Regulations should be adopted.
THEREFORE, IT IS ORDERED, that the proposed regulation to amend Title XIX Medicaid State Plan regarding Home Health Services, specifically, to add accreditation as an option to Medicare certification for Medicaid providers is adopted and shall be final effective November 13, 2018.
Date: 10/24/2018
Kara Odom Walker, MD, MPH, MSHS
Secretary, DHSS
FINAL Attachment 3.1-A
Page 3.1 Addendum
STATE PLAN UNDER TITLE XIX OF THE SOCIAL SECURITY ACT
STATE/TERRITORY: DELAWARE
LIMITATIONS ON AMOUNT, DURATION AND SCOPE OF MEDICAL AND REMEDIAL CARE AND SERVICES
PROVIDED TO THE CATEGORICALLY NEEDY
6.d. 2. Licensed Behavioral Health Practitioner Continued:
Services which exceed the initial pass-through authorization must be approved for re-authorization prior to service delivery. In addition to individual provider licensure, service providers employed by addiction treatment services and co-occurring treatment services agencies must work in a program licensed by the Delaware Division of Substance Abuse and Mental Health (DSAMH) and comply with all relevant licensing regulations. Licensed Psychologists may supervise up to seven (7) unlicensed assistants or post-doctoral professionals in supervision for the purpose of those individuals obtaining licensure and billing for services rendered. Services by unlicensed assistants or post-doctoral professionals under supervision may not be billed under this section of the State Plan. Instead, those unlicensed professionals must qualify under the Early and Periodic Screening, Diagnosis, and Treatment (EPSDT) program or rehabilitation sections of the State Plan or provide services under Home and Community-based authorities.
Inpatient hospital visits are limited to those ordered by the beneficiary's physician. Visits to a nursing facility are allowed for LBHPs if a Preadmission Screening and Resident Review (PASRR) indicates it is a medically necessary specialized service in accordance with PASRR requirements. Visits to Intermediate Care Facilities for Individuals with Mental Retardation (ICF/MR) are noncovered. All LBHP services provided while a person is a resident of an Institute for Mental Disease (IMD) such as a free standing psychiatric hospital or psychiatric residential treatment facility are part of the institutional service and not otherwise reimbursable by Medicaid. Evidence-based Practices require prior approval and fidelity reviews on an ongoing basis as determined necessary by Delaware Health and Social Services (DHSS) and/or its designee. A unit of service is defined according to the Current Procedural Terminology (CPT) or Healthcare Common Procedure Coding System (HCPCS) approved code set consistent with the National Correct Coding Initiative unless otherwise specified.
6. Home Health Services
Home Health agencies must be certified by Medicare or accredited by an accreditation organization and be properly licensed by the State in which they are located.
An "accreditation organization" means a professional organization that evaluates Home Health agencies and certifies that services are being performed in accordance with acceptable practices and standards established by the accreditation organization. A current list of approved accreditation organizations can be found at https://www.nahc.org/consumers-information/home-care-hospice-basics/accrediting-agencies/
FINAL Attachment 4.19-B
Page 6
METHODS AND STANDARDS FOR ESTABLISHING PAYMENT RATES -
OTHER TYPES OF CARE
PAYMENTS FOR MEDICAL AND REMEDIAL CARE AND SERVICES
HOME HEALTH SERVICES
42 CFR 440.70
Home Health Services are reimbursed as follows:
Home Health Services are reimbursed in accordance with 42 CFR 42 CFR 440.70 and when provided as defined in Attachment 3.1-A of this State Plan, subject to the requirements of 42 CFR 441.15 and 42 CFR 441.16.
Home Health agencies must be certified by Medicare and be properly licensed by the State in which they are located.
Payment for Home Health Services shall be reimbursed as follows:
The rates are prospective and are arrayed to determine the seventy-fifth (75th) percentile for each procedure code. The 75th percentile refers to the array of rates with regard to the Delaware Medicaid enrolled providers at the time of the new rate methodology consideration. The rates are then inflated by the four (4) quarter moving average within the CMS Home Health Market Basket Index. The Inflated average cost is per fifteen (15) minutes for each procedure code. Supply cost will be reimbursed as part of the skilled nursing and home health aide prospective rates.
An inflation factor will be applied to the prior year's rates to determine the current year's rates. The inflation indices are obtained from the CMS Home Health Market Basket Index.