DEPARTMENT OF HEALTH AND SOCIAL SERVICES
Division of Medicaid and Medical Assistance
FINAL
ORDER
Inpatient Psychiatric Hospital Services For Individuals Under Age 21
NATURE OF THE PROCEEDINGS:
Delaware Health and Social Services ("Department") / Division of Medicaid and Medical Assistance initiated proceedings to amend Title XIX Medicaid State Plan regarding Inpatient Psychiatric Hospital Services for Individuals under Age 21, specifically, to clarify reimbursement methodology for psychiatric residential treatment facilities (PRTFs). The Department's proceedings to amend its regulations were initiated pursuant to 29 Delaware Code Section 10114 and its authority as prescribed by 31 Delaware Code Section 512.
The Department published its notice of proposed regulation changes pursuant to 29 Delaware Code Section 10115 in the September 2017 Delaware Register of Regulations, requiring written materials and suggestions from the public concerning the proposed regulations to be produced by October 2, 2017 at which time the Department would receive information, factual evidence and public comment to the said proposed changes to the regulations.
SUMMARY OF PROPOSAL
The purpose of this notice is to advise the public that Delaware Health and Social Services (DHSS)/Division of Medicaid and Medical Assistance (DMMA) is proposing to amend Title XIX Medicaid State Plan regarding Inpatient Psychiatric Hospital Services for Individuals under Age 21, specifically, to clarify reimbursement methodology for psychiatric residential treatment facilities (PRTFs).
Statutory Authority
Background
The Psychiatric Services for Individuals under Age 21 benefit at section 1905(a)(16) of the Act, is optional. The benefit must be provided in all States to those individuals who are determined during the course of an Early and Periodic Screening, Diagnosis, and Treatment (EPSDT) screen to need this type of inpatient psychiatric care. Under the EPSDT provision, States must provide any services listed in section 1905(a) of the Act that is needed to correct or ameliorate defects and physical and mental conditions discovered by EPSDT screening, whether or not the service is covered under the State plan.
This benefit, Inpatient Psychiatric Hospital Services for Individuals under Age 21, hereinafter referred to as "Psych under 21," is a service most states have chosen to provide as an optional benefit. Services are provided in psychiatric hospitals or psychiatric units in a hospital, or psychiatric facilities for which states may define accreditation requirements, subject to requirements at 42 CFR 441 Subpart D. Among the requirements for this service is certification of need for inpatient care, and a plan of care for active treatment, developed by an interdisciplinary team.
This benefit is significant as a means for Medicaid to cover the cost of inpatient mental health services. The federal Medicaid program does not reimburse states for the cost of institutions for mental diseases (IMDs) except for young people, who receive this service, and individuals age 65 or older served in an IMD. No later than age 22, individuals are transitioned to community services, or non-Medicaid inpatient services.
Many states provide psych under 21 services through psychiatric residential treatment facilities (PRTFs). A PRTF provides comprehensive mental health treatment to children and adolescents (youth) who, due to mental illness, substance abuse, or severe emotional disturbance, are in need of treatment that can most effectively be provided in a residential treatment facility. All other ambulatory care resources available in the community must have been identified, and if not accessed, determined to not meet the immediate treatment needs of the youth.
PRTF programs are designed to offer a short term, intense, focused mental health treatment program to promote a successful return of the youth to the community. Specific outcomes of the mental health services include the youth returning to the family or to another less restrictive community living situation as soon as clinically possible and when treatment in a PRTF is no longer medically necessary. The residential treatment facility is expected to work actively with the family, other agencies, and the community to offer strengths-based, culturally competent, medically appropriate treatment designed to meet the individual needs of the youth including those identified with emotional and behavioral issues.
To view the Centers for Medicare & Medicaid Services (CMS) Informational Bulletin regarding Inpatient Psychiatric Hospital Services for Individuals under age 21, use the following link:
https://www.medicaid.gov/Federal-Policy-Guidance/downloads/CIB-11-28-12.pdf
Summary of Proposal
Purpose
The purpose of this proposed regulation is to ensure coverage for Inpatient Psychiatric Hospital Services for Individuals under Age 21 by clarifying reimbursement methodologies.
Summary of Proposed Changes
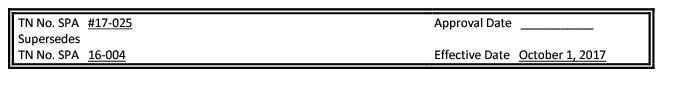
Effective for services provided on and after October 1, 2017 Delaware Health and Social Services/Division of Medicaid and Medical Assistance (DHSS/DMMA) proposes to amend Title XIX Medicaid State Plan to clarify the reimbursement methodologies for Inpatient Psychiatric Hospital Services for Individuals under Age 21.
Public Notice
In accordance with the federal public notice requirements established at Section 1902(a)(13)(A) of the Social Security Act and 42 CFR 447.205 and the state public notice requirements of Title 29, Chapter 101 of the Delaware Code, Delaware Health and Social Services (DHSS)/Division of Medicaid and Medical Assistance (DMMA) gives public notice and provides an open comment period for thirty (30) days to allow all stakeholders an opportunity to provide input on the proposed regulation. Comments were to have been received by 4:30 p.m. on October 2, 2017.
Centers for Medicare and Medicaid Services Review and Approval
The provisions of this state plan amendment (SPA) are subject to approval by the Centers for Medicare and Medicaid Services (CMS). The draft SPA page(s) may undergo further revisions before and after submittal to CMS based upon public comment and/or CMS feedback. The final version may be subject to significant change.
Provider Manuals Update
Also, there may be additional provider manuals that will require small updates as a result of these changes. The applicable Delaware Medical Assistance Program (DMAP) Provider Policy Specific Manuals will be updated. Manual updates, revised pages or additions to the provider manual are issued, as required, for new policy, policy clarification, and/or revisions to the DMAP program. Provider billing guidelines or instructions to incorporate any new requirement may also be issued. A newsletter system is utilized to distribute new or revised manual material and to provide any other pertinent information regarding manual updates. DMAP provider manuals and official notices are available on the Delaware Medical Assistance Provider Portal website: https://medicaid.dhss.delaware.gov/provider
Fiscal Impact Statement
There are no intended content changes other than revised reimbursement methodology. The proposed amendment imposes no increase in cost on the General Fund as the proposed services in this State plan amendment will be budget neutral. The federal fiscal impact associated with this amendment will be zero dollars.
Summary of Comments Received with Agency Response and Explanation of Changes
The State Council for Persons with Disabilities (SCPD) and the Governor's Advisory Council for Exceptional Citizens (GACEC) offered the following summarized observations:
First, both commenters offered grammatical suggestions.
Agency Response: DMMA has revised the policy to include the suggested changes.
Second, both commenters referenced that the deletion of the "add on" for "activities in the plan of care but not in the per diem" is not revenue neutral. And if new third bullet only applied to out-of-state facilities, the deletion creates a lower reimbursement methodology for out-of-state facilities versus in-state facilities. The suggestion was made to amend the new third bullet to authorize an "add on" for "activities in the plan of care but not in the per diem".
Agency Response: DMMA appreciates the comment and agrees with the commenters. The third bullet was revised to include the "add on" for "activities in the plan of care but not in the per diem".
FINDINGS OF FACT:
The Department finds that the proposed changes as set forth in the September 2017 Register of Regulations should be adopted.
THEREFORE, IT IS ORDERED, that the proposed regulation to amend Title XIX Medicaid State Plan regarding Inpatient Psychiatric Hospital Services for Individuals under Age 21, specifically, to clarify reimbursement methodology for psychiatric residential treatment facilities (PRTFs), is adopted and shall be final effective November 11, 2017.
Kara Odom Walker, MD, MPH, MSHS
Secretary, DHSS
FINAL ATTACHMENT 4.9-A.3
STATE PLAN UNDER TITLE XIX OF THE SOCIAL SECURITY ACT
State: DELAWARE
METHODS AND STANDARDS FOR ESTABLISHING PAYMENT RATES
INPATIENT PSYCHIATRIC HOSPITAL SERVICES FOR UNDER [AGE] 21
1. Psychiatric Residential Treatment Facility (PRTF) Reimbursement
Reimbursement for services are based upon a Medicaid fee schedule established by the State of Delaware. Psychiatric
residential treatment facilities will be reimbursed the lesser of:
Except as otherwise noted in the State Plan, the State-developed fee schedule is the same for both governmental and private individual providers and the fee schedule and any annual/periodic adjustments to the fee schedule are published in the Delaware Register of Regulations. The Agency's fee schedule rate was set as of July 1, 2016 and is effective for services provided on or after that date. All rates are published on the Delaware Medical Assistance Program (DMAP) website at www.dmap.state.de.us/downloads/hcpcs.html.
A. Delaware Medicaid per diem PRTF reimbursement rate includes the following covered inpatient psychiatric residential treatment facility (PRTF) activities for individuals under twenty-one years of age when included on the patient's inpatient psychiatric active treatment plan of care:
a. Behavioral Health care by staff who are not physicians
b. Occupational Therapy / Physical Therapy / Speech Therapy
c. Laboratory
d. Transportation
e. Dental
f. Vision
g. Diagnostics/radiology (x-ray)
Starting on 1/1/2019, dental, vision, laboratory, and diagnostics/radiology are excluded from this rate and paid through EPSDT under authority of the 21st Century Cures Act.