DEPARTMENT OF HEALTH AND SOCIAL SERVICES
Division of Medicaid and Medical Assistance
FINAL
ORDER
Prescription Assistance
NATURE OF THE PROCEEDINGS:
Delaware Health and Social Services ("Department") / Division of Medicaid and Medical Assistance initiated proceedings to amend the Delaware Social Services Manual (DSSM regarding Prescription Assistance, specifically, to eliminate the Delaware Prescription Drug Payment Assistance Program. The Department's proceedings to amend its regulations were initiated pursuant to 29 Delaware Code Section 10114 and its authority as prescribed by 31 Delaware Code Section 512.
The Department published its notice of proposed regulation changes pursuant to 29 Delaware Code Section 10115 in the August 2017 Delaware Register of Regulations, requiring written materials and suggestions from the public concerning the proposed regulations to be produced by August 31, 2017 at which time the Department would receive information, factual evidence and public comment to the said proposed changes to the regulations.
SUMMARY OF PROPOSAL
The purpose of this notice is to advise the public that Delaware Health and Social Services (DHSS)/Division of Medicaid and Medical Assistance (DMMA) is proposing to amend the Delaware Social Services Manual (DSSM) Prescription Assistance, specifically, to eliminate the Delaware Prescription Drug Payment Assistance Program.
Statutory Authority
29 Del.C. §6502 Annual estimates of expenditures
Background
The Delaware Prescription Assistance Program (DPAP) was established by the Delaware General Assembly on January 14, 2000, when Senate Bill 6 was passed during the 1999 Legislative Session. DPAP is funded by the Delaware Health Fund and provides prescription and over-the-counter drug coverage to qualified Delaware citizens. In 2007 the Bill was amended to allow the program to pay for the members' Medicare Part D premium. By paying for the premium, clients had access to all of the Medicare drug benefits.
Individuals with Medicare (the majority of DPAP clients) would select a Part D Prescription Drug Plan and apply for Extra Help (Low-Income Subsidy) through the Social Security Administration. The Low-Income Subsidy, or LIS, which is paid by the Centers for Medicare & Medicaid Services, would provide financial assistance (at levels of 100%, 75%, 50%, and 25%) for monthly Part D premiums, annual deductibles, and prescription coverage through the Part D coverage gap to low-income individuals. Medicare Part D would be primary to the Delaware Prescription Assistance Program.
The most recent internal Delaware Health and Social Services/Division of Medicaid and Medical Assistance (DHSS/DMMA) report indicates that all but two members have prescription coverage through Medicare Part D. The program is being eliminated due to a reduction in usage, along with an overall reduction in expenditures by DMMA.
Summary of Proposal
Purpose
The purpose of this proposed regulation is to eliminate the Delaware Prescription Drug Payment Assistance Program.
Summary of Proposed Changes
Effective for services provided on and after July 1, 2017, Delaware Health and Social Services/Division of Medicaid and Medical Assistance (DHSS/DMMA) proposes to amend the Delaware Social Services Manual to eliminate the Delaware Prescription Drug Payment Assistance Program.
Public Notice
In accordance with the federal public notice requirements established at Section 1902(a)(13)(A) of the Social Security Act and 42 CFR 447.205 and the state public notice requirements of Title 29, Chapter 101 of the Delaware Code, Delaware Health and Social Services (DHSS)/Division of Medicaid and Medical Assistance (DMMA) gives public notice and provides an open comment period for thirty (30) days to allow all stakeholders an opportunity to provide input on the proposed regulation. Comments were to have been received by 4:30 p.m. on August 31, 2017.
Provider Manuals Update
The applicable Delaware Medical Assistance Program (DMAP) Provider Policy Specific Manuals will be updated. Manual updates, revised pages or additions to the provider manual are issued, as required, for new policy, policy clarification, and/or revisions to the DMAP program. Provider billing guidelines or instructions to incorporate any new requirement may also be issued. A newsletter system is utilized to distribute new or revised manual material and to provide any other pertinent information regarding manual updates. DMAP provider manuals and official notices are available on the Delaware Medical Assistance Provider Portal website: https://medicaid.dhss.delaware.gov/provider.
Fiscal Impact Statement
The following fiscal savings are projected: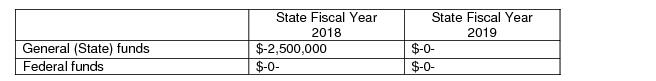
Summary of Comments Received with Agency Response and Explanation of Changes
The State Council for Persons with Disabilities (SCPD) and the Governor's Advisory Council for Exceptional Citizens (GACEC) offered the following summarized observations:
First, SCPD and GACEC commented that it would be informative to disclose what costs the DPAP covered which Medicare-D and the Low-Income Subsidy do not cover.
Agency Response: The DPAP provided coverage for certain Over-the-Counter (OTC) products that are not covered through Medicare Part D. DPAP also provided prescription drug coverage for eligible members during the Part D deductible period and coverage gap, up to the program's $3,000.00 benefit cap per individual per year.
Second, SCPD and GACEC requested additional information on the effect of the repeal.
Agency Response: Effects of the program's termination will vary by individual and may include:
DMMA notified DPAP members about the potential for increased out-of-pocket expenses resulting from the termination of the program. DPAP members were encouraged to consult Medicare to explore options for Part D coverage to help reduce out-of-pocket costs whenever possible.
Third, the SCPD requested "a copy of the last three annual reports prepared pursuant to the recently-repealed 16 Del.C. §3006B."
Agency Response: DMMA provided the requested annual reports.
DMMA is appreciative of the comments from the State Council for Persons with Disabilities and the Governor's Advisory Council for Exceptional Citizens. DMMA is pleased to provide the opportunity to receive public comments and greatly appreciates the thoughtful input given.
FINDINGS OF FACT:
The Department finds that the proposed changes as set forth in the August 2017 Register of Regulations should be adopted.
THEREFORE, IT IS ORDERED, that the proposed regulation to amend the Delaware Social Services Manual (DSSM) regarding Prescription Assistance, specifically, to eliminate the Delaware Prescription Drug Payment Assistance Program, is adopted and shall be final effective November 11, 2017.
Kara Odom Walker, MD, MPH, MSHS,
Secretary, DHSS
30000 Delaware Prescription Assistance Program
30000 Delaware Prescription Assistance Program
30100 Definitions
30200 General Application Information
30201 Disposition of Applications
30202 Timely Determination of Eligibility
30203 Reporting Changes in Circumstances
30300 Technical Eligibility
30301 Citizenship and Alienage
30302 State Residency
30303 Social Security Number
30304 Aged or Disabled Requirement
30305 No Other Prescription Drug Coverage
30305.1 Exceptions to No Other Prescription Drug Coverage
30306 Inmate of a Public Institution
30400 Financial Eligibility
30401 Countable Income
30402 Excluded Income
30403 Eligibility Determination
30404 Effective Date of Coverage
30405 Redetermination of Eligibility
30500 Benefits
30501 Limitations on Benefits
30502 Co-payment Requirement
30503 Waiver of Co-payment for Good Cause
30600 Confidentiality
30601 Release of Information to DPAP Providers
30602 Release of Information to Others
30700 Fair Hearings
The 140th General Assembly amended Title 16, Delaware Code, by adding Chapter 30B to enact the Delaware Prescription Drug Payment Assistance Program. The purpose of this act is to provide payment assistance for prescription drugs and certain Medicare Part D costs to low-income seniors and individuals with disabilities who are ineligible for, or do not have, prescription drug benefits or coverage through federal (excluding Medicare Part D coverage), state, or private sources
The program is administered by the Fiscal Agent under contract with the Delaware Department of Health and Social Services.
The rules in this section set forth the eligibility requirements for coverage under the Delaware Prescription Assistance Program (DPAP). The DPAP is implemented January 1, 2000, with benefits beginning January 14, 2000.
Contractor: the agent who is under contract with the State to administer the DPAP.
Department: the Department of Health and Social Services or DHSS
Division: the Division of Medicaid & Medical Assistance or DMMA
Low Income Subsidy (LIS): Assistance provided by the Centers for Medicare and Medicaid Services to pay Medicare Part D costs for individuals with limited income and resources. The LIS will provide payment assistance with the monthly premium, the yearly deductible, and the coverage gap. The LIS will also provide payment assistance for co-payments after an individual with income below 135% of the Federal Poverty Level reaches a total of $5100 in drug expenses.
Medicare Part D: The Medicare Prescription Drug Program established by the Medicare Prescription Drug, Improvement and Modernization Act of 2003.
Medicare Part D costs: monthly premiums, yearly deductible, and drug costs that fall into the Part D coverage gap.
The application for DPAP must be made in writing on the prescribed form. This request for assistance can be made by the applicant, guardian, or other individual acting for the applicant with his knowledge and consent. The application filing date is the date the application is received in either the Contractor's office or a DSS office.
DPAP will consider an application without regard to race, color, age, sex, disability, religion, national origin, or political belief as per Title VI of the Civil Rights Act of 1964.
Filing an application gives the applicant the right to receive a written determination of eligibility and the right to appeal the written determination.
The Contractor must include in each applicant’s case record facts to support the Contractor's decision on his application. The Contractor must dispose of each application by a finding of eligibility or ineligibility, unless:
a) there is an entry in the case record that the applicant voluntarily withdrew the application, and that the Contractor sent a notice confirming his decision;
b) there is a supporting entry in the case record that the applicant has died; or
c) there is a supporting entry in the case record that the applicant cannot be located.
d) all verification requested is not received by the due date given to the applicant. If all verification requested is not received by the due date, an eligibility determination cannot be made. This will result in denial of the application. Verification that is received and/or provided may reveal a new eligibility issue not previously realized that requires additional verification. If the additional verification requested is not received by the due date given, this will result in denial of the application.
All applicants will receive a notice of acceptance or denial.
A time standard of 45 days will apply. This standard equals the period from the application filing date to the date that the notice of decision is mailed. The standard must be met except in unusual circumstances, such as:
A decision cannot be made because the applicant or his representative delays or fails to take a required action.
There is an administrative or other emergency beyond the Contractor's control.
At time of application and redetermination, each individual must be informed that he is responsible for notifying the Contractor of all changes in his circumstances, which could potentially affect his eligibility for DPAP.
The following requirements are factors of eligibility specific to DPAP.
The individual must be a U.S. citizen or a lawfully admitted alien.
The individual must be living in the State of Delaware.
Each individual applying for DPAP must furnish his or her Social Security number.
The individual must meet one of the following requirements:
a) be age 65 or over, or
b) be an individual between the ages of 19 and 64 who is receiving disability benefits under Title II of the Social Security Act. An individual is considered to meet the "receiving disability benefits" requirement if the individual is a former recipient of either Social Security Disability Insurance benefits or Supplemental Security Income benefits and was required by the Social Security Administration to accept Social Security Survivors benefits.
An individual who is entitled to receive Medicare benefits under Part A or Part B must enroll in Part D in order to be eligible for DPAP. The individual must provide proof of Medicare Part D enrollment.
An individual must apply for the LIS if potentially eligible. The individual must provide a copy of the LIS denial or approval notice.
The individual must not have or must be ineligible for, prescription drug benefits or coverage through federal (excluding Medicare Part D coverage), state, or private sources regardless of any annual limitations to the benefits.
The individual must not have or must be ineligible for:
(a) Medicaid prescription benefits
(b) prescription drug benefits through a third party payer
(c) the Nemours Health Clinic Pharmaceutical benefit as defined on 1/1/99
30307.1 Exceptions to No Other Prescription Drug Coverage
Individuals who are eligible for the following drug benefits will not be excluded from eligibility for DPAP:
(a) individuals eligible for Medicaid as Family Planning Only
(b) individuals covered under a specific disease state insurance program, for example a policy that pays only for cancer drugs
(c) individuals who are members of a discount drug program in which the policy does not actually pay for the drugs, for example American Association of Retired Persons (AARP)
(d) individuals eligible for drug coverage through the Division of Vocational Rehabilitation
(e) individuals eligible for drug coverage through the Division of Substance Abuse, and Mental Health.
(f) individuals covered under Medicare Part D.
An individual who is an inmate of a public institution is not eligible for DPAP.
An individual is an inmate when serving time for a criminal offense or confined involuntarily in State or Federal prisons, jail, detention facilities, or other penal facilities. An individual awaiting trial in a detention center is considered an inmate of a public institution.
Income is any type of money payment that is of gain or benefit to an individual. Income is either counted or excluded for the eligibility determination.
Countable income includes but is not limited to:
1. Social Security benefits – as paid after deduction for Medicare premium
2. Pension – as paid
3. Veterans Administration Pension – as paid
4. U.S. Railroad Retirement Benefits – as paid
5. Wages – net amount after deductions for taxes and FICA
6. Senior Community Service Employment – net amount after deductions for taxes and FICA
7. Interest/Dividends – gross amount
8. Capital Gains – gross amount from capital gains on stocks, mutual funds, bonds.
9. Credit Life or Credit Disability Insurance Payments – as paid
10. Alimony – as paid
11. Rental Income from entire dwelling – gross rent paid minus standard deduction of 20% for expenses
12. Roomer/Boarder Income – gross room/board paid minus standard deduction of 10% for expenses
13. Self Employment – countable income as reported to Internal Revenue Service (IRS)
14. Unemployment Compensation - as paid
Excluded income includes but is not limited to:
1. Annuity payments
2. Individual Retirement Account (IRA) distributions
3. Payments from reverse mortgages
4. Capital gains from the sale of principal place of residence
5. Conversion or sale of a resource (i.e. cashing a certificate of deposit)
6. Income tax refunds
7. Earned Income Tax Credit (EITC)
8. Vendor payments (bills paid directly to a third party on behalf of the individual)
9. Government rent/housing subsidy paid directly to individual (i.e. HUD utility allowance)
10. Loan payments received by individual
11. Proceeds of a loan
12. Foster care payments made on behalf of foster children living in the home
13. Retired Senior Volunteer Program (RSVP)
14. Veterans Administration Aid and Attendance payments
15. Victim Compensation payments
16. German reparation payments
17. Agent Orange settlement payments
18. Radiation Exposure Compensation Trust Fund payments
19. Japanese-American, Japanese-Canadian, and Aleutian restitution payments
20. Payments from long term care insurance or for inpatient care paid directly to the individual
To be eligible for DPAP:
(a) the individual must have countable income that is less than 200% of the Federal Poverty Level, or
(b) the individual has countable income that is equal to or greater than 200% of the Federal Poverty Level and the individual has prescription drug expenses that exceed 40% of his countable income.
The Federal Poverty Level (FPL) is published annually. The income eligibility standard based on the FPL will be issued within 10 business days after the FPL is published. The revised income eligibility standard will be used to determine eligibility for the month following the month in which the standard is issued.
Coverage begins on the first day of the month following the month that eligibility is determined. There is no retroactive coverage. Eligible individuals will receive an identification card for DPAP.
A redetermination of eligibility must be completed by June 30 of each year. If an individual’s initial coverage begins in April, May or June, a redetermination will not be required until June of the following year. A redetermination is a re-evaluation of a recipient’s continued eligibility for DPAP coverage. In a redetermination, all eligibility factors are re-examined to ensure that the recipient continues to meet eligibility requirements. When a redetermination is due, the recipient is required to complete and return a new DSS application form. Failure to complete and return a DSS application form will result in termination of eligibility. A redetermination is complete when all eligibility factors are examined and a decision regarding continued eligibility is reached.
DPAP coverage will be terminated when the Contractor or DSS is notified by the recipient that he or she no longer wants coverage.
Prescription drugs covered under DPAP are restricted to medically necessary products manufactured by pharmaceutical companies that agree to provide manufacturer rebates. Policy and guidelines will follow the existing Delaware Medical Assistance Program limitations. Services covered include generic and brand name prescription drugs that have been approved as safe and effective by the Federal Food and Drug Administration as well as cost effective over-the-counter drugs prescribed by a practitioner. Necessary diabetic supplies not covered by Medicare will also be covered. Medications that are covered by Medicare are not covered under DPAP.
30500.1 Benefits for Individuals with Medicare Part D Coverage
DPAP will provide payment assistance for Medicare Part D monthly premiums, yearly deductible, those drug costs that fall into the Part D coverage gap, and drugs that are excluded from Medicare Part D.
Medicare Part D coverage will be primary to payment assistance under DPAP.
Payment assistance to each eligible individual shall not exceed $3,000.00 per benefit year. Individuals will receive a notice when 75% of the $3,000.00 cap has been expended.
There is a co-payment of $5.00 or 25% of the cost of the prescription whichever is greater. The pharmacy will not dispense or provide the prescription until the co-payment is collected.
30502.1 Co-payment Requirement for Individuals with Medicare Part D Coverage
There is a co-payment of $5.00 or 25% of the cost of the prescription (whichever is greater) during the Part D deductible and coverage gap and for drugs that are excluded from Part D. DPAP will not provide payment assistance for Medicare Part D co-payments. When the individual receives a prescription drug that is covered under Medicare Part D, the individual is responsible for the Medicare Part D co-payment.
At the written request of the individual, the co-pay requirement may be waived for good cause.
Good cause for waiver of the co-payment is:
The individual has experienced a catastrophic situation resulting in unexpected, extraordinary expenses related to loss or significant damage to shelter or the well being of the individual or his immediate family.
The written request must explain the circumstances that led to the request. Verification of the circumstances is required in the form of collateral evidence that may include, but is not limited to, repair bills and police or insurance reports. The DPAP will provide written notification to the individual regarding the good cause decision. If good cause is granted, the co-payments will be waived for the remainder of the fiscal year.
DPAP will provide safeguards that restrict the use or disclosure of information about applicants and recipients to purposes directly connected with the administration of the DPAP.
Purposes directly related to administration of the DPAP include establishing eligibility, providing services for recipients, determining the amount of medical assistance, and conducting or assisting an investigation, prosecution, or civil or criminal proceeding related to the administration of the program.
At a minimum, the types of information about applicants and recipients that must be safeguarded and not released without consent include:
Names and addresses;
Medical services provided;
Social and economic conditions or circumstances;
Contractor evaluation of personal information;
Medical data, including diagnosis and past history of disease or disability;
Information received for verifying income eligibility and amount of medical assistance payments; and
Information about third party liability.
DPAP providers have a contractual obligation to safeguard information about recipients. Providers may have access to certain eligibility information if they can provide:
a DPAP identification number, or
two of the following identifying factors: individual's full name, date of birth, Social Security number;
AND
the date of service.
Providers who supply the above identifying factors may be given the following information:
a) correct spelling of the recipient's name;
b) DPAP number;
c) date of birth;
d) an indication whether the individual is eligible for the date of service given or for a range of dates given. Providers may not be given all periods of eligibility.
At the time of application, individuals are informed that all eligibility information is confidential and disclosure without written permission of the individual is limited. DPAP has the authority to responsibly share information concerning applicants and recipients with:
a) DHSS employees;
b) Federal or federally assisted programs that provide assistance to individuals on the basis of need (SSI, HUD);
c) contracted service providers
Information may be released to comply with a subpoena or other valid court order.
DPAP must obtain specific written permission from the individual before releasing information to any other persons or sources.
A fair hearing is an administrative hearing held in accordance with the principles of due process. An opportunity for a fair hearing will be provided, subject to the provisions in policy at DSSM 5000 - 5607.







