department of health and social services
Division of Medicaid and Medical Assistance
PROPOSED
PUBLIC NOTICE
Non-Emergency Medical Transportation Services
In compliance with the State's Administrative Procedures Act (APA - Title 29, Chapter 101 of the Delaware Code) and under the authority of Title 31 of the Delaware Code, Chapter 5, Section 512, Delaware Health and Social Services (DHSS) / Division of Medicaid and Medical Assistance (DMMA) is proposing to amend the Delaware Title XIX Medicaid State Plan regarding Non-Emergency Medical Transportation Services.
Any person who wishes to make written suggestions, compilations of data, testimony, briefs or other written materials concerning the proposed new regulations must submit same to Sharon L. Summers, Planning & Policy Development Unit, Division of Medicaid and Medical Assistance, 1901 North DuPont Highway, P.O. Box 906, New Castle, Delaware 19720-0906 or by fax to 302-255-4425 by June 30, 2010.
The action concerning the determination of whether to adopt the proposed regulation will be based upon the results of Department and Division staff analysis and the consideration of the comments and written materials filed by other interested persons.
SUMMARY OF PROPOSAL
The proposed provides notice to the public that the Division of Medicaid and Medical Assistance (DMMA) intends to amend the Title XIX Medicaid State Plan to implement the provisions of Section 6083 of the Deficit Reduction Act (DRA) of 2005 (Public Law 109-171) regarding Non-Emergency Medical Transportation Services.
Statutory Authority
Background
Section 6083 of the DRA amends section 1902(a) of the Social Security Act by adding a new section 1902(a)(70) that provides States the authority to establish, under the State plan, a non-emergency medical transportation (NEMT) brokerage program.
Medicaid programs are federally required in their Title XIX Medicaid state plans to ensure necessary transportation to and from providers. Federal regulations, at both §§431.53 and 440.170(a), permit this coverage in either of two ways, at the state's discretion: 42 CFR §431.53 permits coverage as an administrative expense; 42 CFR §440.170 permits transportation coverage as a medical expense under its State Medicaid plan. Besides the differences in federal financial participation (FFP) for this service for some states (the medical expense is federally reimbursed higher), the most significant difference in these two alternatives is the amount of service coordination and management that is permitted by 42 CFR §431.53.
Prior to enactment of the DRA, when a State elected to provide transportation as medical assistance under its State plan, the State needed to receive a waiver under 1915(b) of the Act in order to institute a NEMT brokerage program.
The law has changed. States are no longer required to obtain a section 1915(b) waiver in order to provide NEMT as an optional medical service through a contracted broker. Under section 1902(a)(70), a State may now use a NEMT brokerage program when providing transportation as medical assistance under the State plan.
Summary of Proposal
The Delaware Medical Assistance Program (DMAP) has a non-emergency medical transportation brokerage program in place as an "administrative service". This amendment establishes DMAP's non-emergency medical transportation brokerage program in the State's Title XIX state plan pursuant to Section 6083 of the Deficit Reduction Act of 2005. This approach will allow for coverage of non-emergency medical transportation through a contracted broker as a medical service comparable to other medical services DMAP covers such as physician and hospital care.
The proposed amendment simultaneously repeals State plan language relating to transportation cost-sharing for Medicaid recipients. There will be no client co-payment requirement for non-emergency medical transportation services.
An approved state plan amendment will allow DMAP to continue to utilize a transportation broker for meeting the non-emergency transportation needs of Medicaid recipients.
The provisions of this amendment are effective July 1, 2010 and subject to approval by the Centers for Medicare and Medicaid Services (CMS).
DMMA PROPOSED REGULATION #10-27a
REVISIONS:
Revision: CMS ATTACHMENT 3.1-A
OMB No. Page 9a
STATE PLAN UNDER TITLE XIX OF THE SOCIAL SECURITY ACT
State/Territory DELAWARE
AMOUNT, DURATION, AND SCOPE OF MEDICAL AND REMEDIAL CARE
AND SERVICES PROVIDED TO THE CATEGORICALLY NEEDY
24. Any other medical care and any other type of remedial care recognized under State law and specified by the Secretary.
a 1. Transportation (provided in accordance with 42 CFR 440.170 as an optional medical service).
Non-emergency medical transportation is provided statewide through a brokerage program as an optional medical service in accordance with 1902(a)(70) of the Social Security Act and 42 CFR 440.170(a)(4) and all other requirements relating to Medicaid services.
a 2. Brokered Transportation 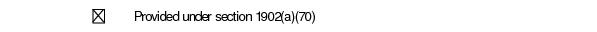
The State assures it has established a non-emergency medical transportation program in order to more cost-effectively provide transportation, and can document, upon request from CMS, that the transportation broker was procured in compliance with the requirements of 45 CFR 92.36 (b)-(f).
(1) The State will operate the broker program without the requirements of the following paragraphs of section 1902(a);
Revision: CMS ATTACHMENT 3.1-A
OMB No. Page 9a.1.
STATE PLAN UNDER TITLE XIX OF THE SOCIAL SECURITY ACT
State/Territory DELAWARE
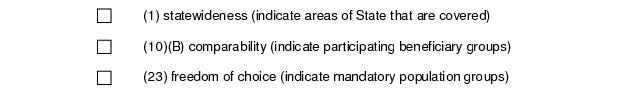
(2) Transportation services will include: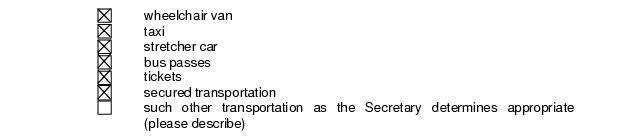
(3) The State assures that transportation services will be provided under contract with a broker who:
(i) is selected through a competitive bidding process based on the State's evaluation of the broker's experience, performance, references, resources, qualifications, and costs;
(ii) has oversight procedures to monitor beneficiary access and complaints and ensures that transport personnel are licensed, qualified, competent, and courteous;
(iii) is subject to regular auditing and oversight by the State in order to ensure the quality of the transportation services provided and the adequacy of beneficiary access to medical care and services;
(iv) complies with such requirements related to prohibitions on referrals and conflict of interest as the Secretary shall establish (based on prohibitions on physician referrals under section 1877 and such other prohibitions and requirements as the Secretary determines to be appropriate);
Revision: CMS ATTACHMENT 3.1-A
OMB No. Page 9a.2.
STATE PLAN UNDER TITLE XIX OF THE SOCIAL SECURITY ACT
State/Territory DELAWARE
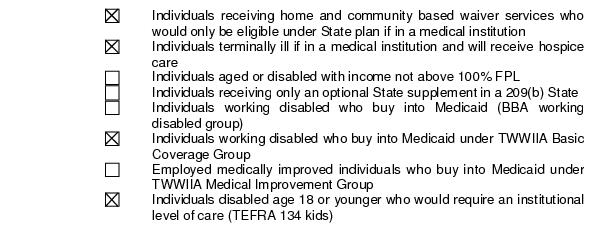
(4) The broker contract will provide transportation to the following categorically needy mandatory populations:
(5) The broker contract will provide transportation to the following categorically
needy optional populations:
Revision: CMS ATTACHMENT 3.1-A
OMB No. Page 9a.3.
STATE PLAN UNDER TITLE XIX OF THE SOCIAL SECURITY ACT
State/Territory DELAWARE
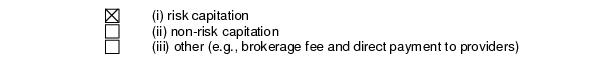
(6) The State will pay the contracted broker by the following method:
Effective Date:
DELAWARE will implement this State plan amendment on July 1, 2010.
DMMA PROPOSED REGULATION #10-27b
REVISIONS:
STATE PLAN UNDER TITLE XIX UNDER THE SOCIAL SECURITY ACT ESTABLISHMENT AND MAINTENANCE OF STATE AND FEDERAL STANDARDS
STATE OF DELAWARE
ATTACHMENT 3.1-D
METHODS OF PROVIDING TRANSPORTATION
Transportation is covered as administrative service through a broker system provided statewide through a brokerage program as an optional medical service in accordance with 1902(a)(70) of the Social Security Act, 42 CFR 440.170(a)(4) and all other requirements relating to Medicaid services.
DMMA Proposed Regulation #10-27c
REVISIONS:
ATTACHMENT 4.18-A
Page 1
STATE PLAN UNDER TITLE XIX OF THE SOCIAL SECURITY ACT
STATE: DELAWARE
A. The following charges are imposed on the categorically needy for services other than those provided under section 1905 (a) (1) through (5) and (7) of the Act:
Service | Type of Charge | Amount and Basis for Determination | ||
Deductible | Coinsurance | Co-payment | ||
1.Non-Emergency Medical Transportation 2. Pharmacy | -0- -0- | -0- -0- | $1.00 per one-way trip X | 1. This co-payment is effective October 1, 2002 and is based on the ranges specified in 42 CFR §§44754 and 447.55. 2. This co-payment is effective January 10, 2005 and is based upon the cost of the drug as follows: Medicaid Payment for the Drug Co-payment $10.00 or less $ .50 $10.01 to $25.00 $1.00 $25.01 to $50.00 $2.00 $50.01 or more $3.00 |
ATTACHMENT 4.18-A
Page 2
STATE PLAN UNDER TITLE XIX OF THE SOCIAL SECURITY ACT
STATE: DELAWARE
B. The method used to collect cost sharing charges for categorically needy individuals:
X Providers are responsible for collecting the cost sharing charges from individuals
The agency reimburses providers the full Medicaid rate for services and collects the cost sharing charges from individuals.
C. The basis for determining whether an individual is unable to pay the charge, and the means by which such an individual is identified to providers, is described below:
Non-Emergency Transportation (NET) Co-payment
Non-Emergency Transportation (NET) is provided as an administrative activity under the State Plan. The State's position is that as an administrative activity, NET co-payment requirements are not subject to 42 CFR 447.53(b), exclusions from cost-sharing.
The Transportation Broker or Transportation Provider will, based on information available to them, make a determination of the client's ability to pay the co-payment. Non-payment of this standard cost-sharing amount may result in denial of the service at the Transportation Broker's or Transportation Provider's discretion. Providers may voluntarily provide transportation to client who cannot pay the co-payment amount, however the State will not reimburse the Transportation Broker or the Transportation Provider any co-payment amounts for which the client is or would have been liable. Further, the Transportation Broker or Transportation Provider have complete discretion as to whether they will pursue any unpaid co-payment amounts from clients who were provided non-emergency transportation but failed to reimburse the Transportation Provider the required co-payment fee at the time of the service. The State will not pursue unpaid co-payment amounts from clients.
Pharmacy Services Co-payment
The Pharmacy (Pharmacist) Provider will be advised via the Point-of-Sale System regarding the client's liability for the drug co-payment and the amount of the co-payment. When a client advises a pharmacy of an inability to pay the applicable co-payment amount at the time the prescription is filled, the pharmacy cannot refuse to fill the prescription and must dispense the drug as prescribed.
The client will remain liable for reimbursement of the co-payment amount and will be responsible for paying the pharmacy when financially able. Medicaid will not pay the co-payment amount to the pharmacy where a client declares an inability to pay. Provider payment will continue to be that sum which is the Medicaid fee minus the applicable client co-payment amount.
ATTACHMENT 4.18-A
Page 3
STATE PLAN UNDER TITLE XIX OF THE SOCIAL SECURITY ACT
STATE: DELAWARE
D. The procedures for implementing and enforcing the exclusions from cost sharing contained in 42 CFR 447.53 (b) are described below:
Exclusions from cost sharing requirements are programmed into the Medicaid Management Information System and the Point-of-Sale (POS) System.
Providers are informed about applicable service and amount; and, the prohibition of service denial if client is unable to meet the co-pay amount by the following methods: (1) provider manuals, which are distributed to all providers; (2) DMAP website; and (3) provider newsletters.
Co-payment requirements are set forth in provider manuals, which are distributed, to all providers. The billing instructions are updated and transmitted to providers via the Provider Newsletter. These instructions are incorporated in the billing instruction section of the provider manuals, which are given to all providers.
E. Cumulative maximums on charges: See descriptions below:
X For Non-Emergency Transportation (NET) Co-payment, the State policy does not provide maximums.
X For Pharmacy Services Co-payment, cumulative maximums have been established as described below:
$15.00 cumulative monthly maximum co-payment amount aggregated for pharmacy services. Once a client has met the individual monthly maximum co-payment for his or her prescriptions, the Point of Sale (POS) System will NOT indicate a co-payment is due. Medicaid will keep track of the cumulative number of prescriptions for a client with co-payments. Any prescriptions dispensed after the cumulative maximum monthly co-payment amount is met are not subject to a co-payment. Reversal of a previously filled prescription with a co-payment will require a refund of the co-payment to the individual, and will cause the next prescription filled for that client to be adjudicated with a co-payment.
13 DE Reg. 1504 (06-01-10) (Proosed)







