DELAWARE HEALTH INFORMATION NETWORK
PROPOSED
PUBLIC NOTICE
103 Delaware Health Care Claims Database Data Collection Regulation
Agency: Delaware Health Information Network
Contact: Dr. Jan Lee
Chief Executive Officer
(302)678-0220
Submit Comments by email to info@dhin.org by July 31, 2017
Title of Proposed Regulation: Delaware Health Care Claims Database Data Collection Regulation
Summary of the Regulation:
This regulation supports implementation of 16 Del.C. Ch. 103, Subchapter II, The Delaware Health Care Claims Database. It summarizes the requirements for submission of claims data by a mandatory reporting entity, to include a reporting schedule and a template for a data submission and use agreement to be entered into between DHIN and each reporting entity. The agreement includes procedures for submission, collection, aggregation, and distribution of claims data, and a summary of how claims data may be used for geographic, demographic, economic, and peer group comparisons.
Sub-regulatory technical guidance may be found on the DHIN web site in the form of a Data Submission Guide.
103 Delaware Health Care Claims Database Data Collection Regulation
1.1 Statutory Authority. 16 Del.C. §10306 authorizes DHIN to promulgate rules and regulations to carry out its objectives under 16 Del.C. Ch. 103, Subchapter II.
1.2 The Health Care Claims Database ("HCCD") was created by statute, pursuant to 16 Del.C. Ch. 103, Subchapter II, under the purview of DHIN, to achieve the "Triple Aim" of the State's ongoing health care innovation efforts: (1) improved health; (2) health care quality and experience; and (3) affordability for all Delawareans. The HCCD is created and maintained by the Delaware Health Information Network (DHIN), to facilitate data driven, evidence-based improvements in access, quality, and cost of healthcare and to promote and improve the public health through increased transparency of accurate Claims Data and information. To accomplish those objectives, a centralized Health Care Claims Database was established to enable the State to more effectively understand utilization across the continuum of health care in Delaware and achieve the Triple Aim.
The following words, terms, and phrases, when used in this regulation, shall have the following meaning, and use of the singular shall include the plural, unless the context clearly indicates otherwise:
"Claims data" includes required claims data and any additional health care information that a voluntary reporting entity elects, through entry into an appropriate Data Submission and Use Agreement, to submit to the Delaware Health Care Claims Database.
"Data Submission and Use Agreement" or "DSUA" shall mean the agreement between the HCCD Administrator and the Reporting Entity describing the specific terms and conditions for data submission and use. A template for the DSUA is Attachment B to this regulation.
"HCCD Administrator" shall mean the Delaware Health Information Network and its staff and contractor(s) that are responsible for collecting data submissions, providing secure production services and providing data access for approved users.
"Health Care Claims Database" or "HCCD" shall mean the database and associated technology components maintained by DHIN and authorized under 16 Del.C. Ch. 103, Subchapter II.
"Health Care Claims Database Committee" or the "Committee" shall mean the subcommittee established by the Delaware Health Information Network Board of Directors and governed by its by-laws that has the authority to determine when claims data should be provided to a Data Requester to facilitate the purposes of the enabling legislation, and such other duties as designated the DHIN Board of Directors consistent with the enabling legislation.
"Health care services" means as defined in 18 Del.C. §6403.
"Health insurer" shall mean as defined in 18 Del.C. §4004(b). "Health insurer" does not include providers of casualty insurance, as defined in 18 Del.C. §906; providers of group long-term care insurance or long-term care insurance, as defined in 18 Del.C. §7103; or providers of a dental plan or dental plan organization, as defined in 18 Del.C. §3802.
"Mandatory Reporting Entity" means the following entities, except as prohibited under federal law:
"Member" means individuals, employees, and dependents for which the Reporting Entity has an obligation to adjudicate, pay or disburse claims payments. The term includes covered lives. For employer-sponsored coverage, Members include certificate holders and their dependents. This definition includes all members of the State Group Health Insurance Program regardless of state of residence.
"Provider" means a hospital, facility, or any health care practitioner licensed, certified, or authorized under State law to provide Health Care Services and includes hospitals and health care practitioners participating in group arrangements, including accountable care organizations, in which the hospital or health care practitioners agree to assume responsibility for the quality and cost of health care for a designed group of beneficiaries.
"Pricing information" includes the pre-adjudicated price charged by a Provider to a Reporting Entity for Health Care Services, the amount paid by a Member or insured party, including co-pays and deductibles, and the post-adjudicated price paid by a Reporting Entity to a Provider for Health Care Services.
"Reporting Date" means a calendar deadline for test, historical and periodic update file submission to be scheduled on a regularly recurring basis, by which Required Claims Data must be submitted by a Reporting Entity to the Health Care Claims Database, as shown in the Data Submission Guide.
"Reporting Entity" means either a Mandatory Reporting Entity or a Voluntary Reporting Entity.
"Required Claims Data" as authorized under 16 Del.C. §10312(8) shall mean the required data containing records of member eligibility, medical services claims and pharmacy claims as specified in the Submission Guide.
"Submission Guide" shall mean the document providing the specific formats, timelines, data quality standards and other requirements for claims data submission, incorporated as Addendum One to the DSUA. It shall be established and maintained as technical guidance document and substantively updated on an annual basis.
"Third Party Administrator" means as defined in 18 Del.C. §102.
"Voluntary Reporting Entity" includes any of the following entities that has chosen to submit or has been instructed to submit data at the request of an employer or client and enters into a Data Submission and Use Agreement, unless such entity is a Mandatory Reporting Entity:
3.1 Registration: By December 31 of each year, each Mandatory Reporting Entity and each Voluntary Reporting Entity shall provide a contact and enrollment update form indicating if health care claims are being paid for Members and if applicable the types of coverage and estimated enrollment for the following calendar year. Each Mandatory Reporting Entity and participating Voluntary Reporting Entity is responsible for resubmitting or amending the form whenever modifications occur relative to the health care data files, type(s) of business conducted, or contact information.
3.2 Threshold for Covered Lives: Mandatory Reporting Entities with fewer than a total of 1000 covered lives may request an exemption from data submission at the end of a calendar year for the next year. If total enrollment subsequently increases to more than 1000 covered lives, the Mandatory Reporting Entity shall notify the HCCD Administrator to develop a compliance schedule. A Mandatory Reporting Entity that becomes eligible for an exemption shall continue to submit data for two full calendar quarters after receiving such exemption.
3.3 Excluded Mandatory Reporting Entities: As defined in 16 Del.C. §10312(3), the following providers of coverage are excluded from this rule: casualty insurance, long term care, dental care vision care, and employee welfare benefit plans regulated by ERISA.
3.4 Participating Voluntary Entities: Voluntary Reporting Entities are held to the same standards, expectations, and processes as Mandatory Reporting Entities for as long as they remain Reporting Entities.
3.5 New Reporting Entities that have not previously submitted files to the HCCD shall notify the HCCD Administrator and shall submit files according to the form and intervals described in Attachment A "Reporting Schedule."
3.6 Run-Out Period After Terminating Coverage: Mandatory Reporting Entities shall submit medical and pharmacy claims files for at least six months following the termination of coverage date for any Member for any reason, including a change in the status of the Reporting Entity. This should include any subrogated claims or claims held in suspense, with dates of service up to and including the termination date.
4.1 Data Submission and Use Agreement: Reporting Entities shall enter into the HCCD Data Submission and Use Agreement, or "DSUA," no later than 90 days after the effective date of this rule. Such agreement shall be incorporated into this regulation as Attachment B.
4.2 Submission Guide: The HCCD Administrator shall develop and disseminate a Submission Guide, included as Addendum One to the DSUA. All files must conform to the formats and data quality requirements established in the Submission Guide, generally as follows:
4.3 Submission Schedule: Reporting Entities shall submit data files pursuant to the schedule in Attachment A.
4.4 Data Submitter Responsibilities: Each Reporting Entity is responsible for the submission of all Required Claims Data processed by any subcontractor on its behalf unless such subcontractor is already submitting the identical Required Claims Data as a Reporting Entity.
4.4.1 Upon notification by the HCCD Administrator, Reporting Entities shall provide corrected, conforming files within 10 business days. The HCCD Administrator may grant extensions of deadlines.
4.4.2 The HCCD Administrator may grant temporary or permanent approvals of a Reporting Entity's request for an override of a data submission requirement.
4.5 Replacement of Data Files. No Reporting Entity may replace a complete data file submission more than one year after the end of the month in which the file was submitted unless it can establish exceptional circumstances for the replacement. Any replacements after this period must be approved by the HCCD Administrator. Individual adjustment records may be submitted with any monthly data file submission.
4.6 Updating Submission Guide: The HCCD Administrator may update reporting specifications annually. Reporting Entities shall submit data that conforms to the updated specifications within 180 days after the effective date of the new version of the Submission Guide.
4.7 Submitting Additional Information: The HCCD Administrator may require Reporting Entities to submit information about the insurance product covering each member, including covered services, market sector, plan characteristics, total premiums, deductibles, co-insurance and copayments, by amending the Submission Guide.
5.1 Pursuant to 29 Del.C. §10002(I)(1), medical and other health care data on individual persons is not a Public Record under the Freedom of Information Act.
5.2 All claims data shall be transmitted to the HCCD Administrator and stored in a secure manner compliant with the Security Rule of the Health Insurance Portability and Accountability Act (HIPAA) of 1996 and the Health Information Technology for Economic and Clinical Health Act (HITECH) of 2009, as each is amended from time to time.
5.3 Transmission, storage and use or disclosure of claims data shall conform to all applicable Federal and State laws and regulations which address privacy, security, confidentiality, and breach notification of health care data.
Compliance: Mandatory Reporting Entities' failure to file, report or correct data or comply with data standards may be considered a violation of 16 Del.C. Ch. 103.
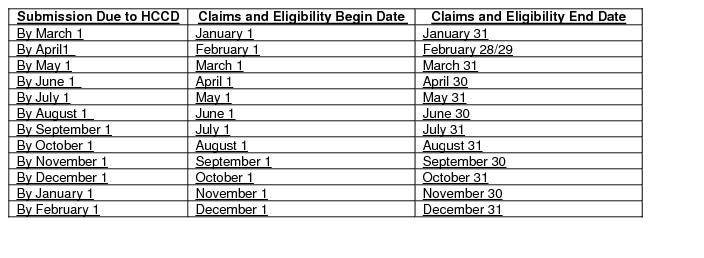
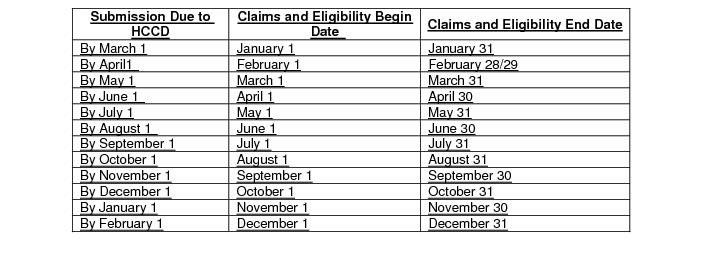
Attachment A
Reporting Schedule
1. Test Files
Reporting Entities shall submit one month of Required Claims Data files containing Member, Claims, Prescription Drugs and a sample of Provider data not more than 180 days after the effective date of this rule or as otherwise approved by the HCCD Administrator.
2. Historical Files
Reporting Entities shall submit Required Claims Data files for calendar years 2013, 2014, 2015 and 2016 that conform to file formats on the 181st day after the effective date of this rule.
3. Partial year submission for the current calendar year
Reporting Entities shall submit Claims Data files for calendar 2017 and for claims adjudicated in the elapsed months of calendar 2018, as directed by the HCCD Administrator, no later than May 1, 2018.
4. Ongoing Data Submission
Reporting Entities shall submit monthly files containing claims paid and encounters adjudicated during the prior calendar month within 30 calendar days of the last day of the following month. The schedule for this submission is provided below and will continue in similar format in subsequent years. Submission dates falling on a weekend or legal holiday are extended to the next following business day.
Attachment B
Data Submission and Use Agreement Template
Data Submission and Use Agreement
Between the Delaware Health Information Network
and
[name of Reporting Entity]
For the Delaware Health Care Claims Database
This Data Submission and Use Agreement between the Delaware Health Information Network ("DHIN"), a not-for-profit statutory instrumentality of the State of Delaware located at 107 Wolf Creek Blvd, Suite, 2, Dover, DE 19901 and [name of reporting entity] (the "Reporting Entity") sets forth the terms and conditions for the collection and use of health care claims data for the Delaware Health Care Claims Database.
Recitals
WHEREAS Under 16 Del.C. Ch. 103 as enacted, the Delaware General Assembly directed the Delaware Health Information Network to develop, maintain and administer the Delaware Health Care Claims Database (HCCD); and
WHEREAS Effective health care data analysis and reporting are essential to achieving the Triple Aim and helping move the state's health care system from a fee-for-service to a valued-based system that rewards providers for quality and efficiency of care; and
WHEREAS Claims data are an important component of population health research and analysis and support value-based health care purchasing and prevalence of illness or injury; and
WHEREAS provider and other health care entities accepting financial risk for managing the health care needs of a population should have access to claims data as necessary to effectively manage that risk; and
WHEREAS DHIN Is authorized to create the HCCD to facilitate data-driven, evidence-based improvements in health care and improve public health through increased transparency of accurate health care claims data and information; and
WHEREAS 16 Del.C. §10313 directs that DHIN and each reporting entity shall execute a data submission and use agreement that includes procedures for submission, collection, aggregation and distribution of claims data,
NOW THEREFORE THE PARTIES AGREE AS FOLLOWS:
1. Precedence
a. DHIN shall promulgate regulations to implement the provisions of 16 Del.C. Ch. 103, hereinafter, and as the same may be amended from time to time, the "HCCD Regulations". The HCCD Regulations shall take precedence over any terms and conditions represented in this Agreement.
b. Definitions in Section 2.0 of the HCCD Regulations shall also pertain to this Agreement.
2. Data Submission: Privacy and Security
a. 16 Del.C. Ch. 103 establishes DHIN as a public health authority that is responsible for public health matters pursuant to 45 CFR 164.501.
b. The HIPAA Privacy Rule permits covered entities to disclose PHI for general public health activities per 45 CFR 164.512(b)(1)(i).
c. Notwithstanding these provisions, DHIN shall ensure protection of patient privacy under provisions of 16 Del.C. Ch. 103, and including HIPAA, Title XIX and XXI of the Social Security Act and the HITECH Act and all other applicable state and federal privacy laws.
3. Data Submission: Collection
a. Reporting Entities shall submit Required Claims Data to the HCCD according to the specifications set forth in the Submission Guide. The Submission Guide is a technical guidance document, and may be updated and replaced without replacing the entire agreement.
b. Reporting Entities shall submit Required Claims Data to the HCCD according to the schedule set forth in Attachment A, Reporting Schedule, of the HCCD Regulations, or as mutually agreed. The schedule is included herein for convenience, but in case of conflict between this Agreement and the HCCD Regulations, the HCCD Regulations shall take precedence.
c. Reporting entities shall submit data files using protocols developed by the HCCD.
i. The Submission Guide shall reflect the content and formats in use by similar databases in other states.
ii. The data submission specifications shall be updated no more than once per calendar year.
iii. The parties agree to review and discuss any such changes prior to the effective date.
iv. Reporting Entities shall provide conforming data no later than 180 calendar days after publication of changes or by agreement between the HCCD Administrator and the Reporting Entity.
v. The HCCD Administrator may provide clarifications and technical corrections as needed to assist Reporting Entities in providing data submissions that conform to specifications.
d. Reporting entities shall provide corrected data files within the timelines established in subsection 4.4.1 of the HCCD Regulations, or as mutually agreed.
e. Upon agreement between DHIN and the Reporting Entity, the Reporting Entity may submit additional data to the HCCD to improve or augment established reporting.
f. DHIN will review the Submission Guide and any subsequent annual revisions with Reporting Entities prior to the 180 day implementation period and on an annual basis thereafter.
g. Data collection methodologies in the Submission Guide shall facilitate uniformity among various health care claims databases of other states and specification of data fields, consistent with national standards.
h. Reporting Entities may request exemptions from specific data collection requirements, including minimum standards for reporting, subject to the approval of the HCCD Administrator.
4. Claims Data Uses
a. Pursuant to 16 Del.C. §10314(a)(1), Claims Data shall only be provided to a requesting party when a majority of the HCCD Committee determines that such request facilitates the statutory purposes of the HCCD.
i. Reporting Entities shall be given opportunity for comment prior to release of Claims Data.
ii. Determinations of the Committee shall be provided in writing to the requesting party.
iii. Decisions of the Committee shall be final and not subject to appeal.
b. Data Requestors may include payers, providers and purchasers.
c. The submitted claims data may be used for the broad purposes described in the enabling statute, including:
i. Alternative delivery and payment models
ii. Population health research
iii. Provider risk-sharing arrangements
iv. Public transparency
v. Other uses in furtherance of the "Triple Aim" of improved health, health care quality and experience, and affordability
d. Detailed permitted uses include, but are not limited to, the following:
i. Population health research and reporting on disease incidence, prevalence, and geographic distribution, costs of care and service utilization
ii. Health care service price variation reports and studies
iii. Design, model and evaluate payment models and purchasing initiatives
iv. Effects of care delivery strategies (e.g., care coordination, behavioral health integration) on utilization and outcomes
v. Efficiency of care, service models or procedures based on quality, value and/or outcomes
vi. Public facing provider performance reports
vii. Augment patient-specific records with data derived from the HCCD to improve the care of the patient, ensure better outcomes and deliver better value.
e. Publicly available data and reports shall, to the fullest extent practicable, comply with guidance in Statement 6 of the United States Department of Justice and Federal Trade Commission Enforcement Policy on Provider Participation in Exchanges of Price and Cost Information, August 1996, as the same may be amended, supplemented or modified from time to time, available at https://www.justice.gov/atr/statements-antitrust-enforcement-policy-health-care#CONTNUM_49 (last visited June 5, 2017).
f. Standard public-facing reports may be developed which provide aggregated, summary level views of the data in accordance with the statutory purpose of public transparency.
Applicable Law:
This Agreement shall be governed by and construed under the laws of the State of Delaware without regard to conflicts of law principles.
IN WITNESS WHEREOF, and intending to be legally bound thereby, the Parties have caused their duly authorized representatives to execute this Agreement.
Signatories:
[Reporting Entity] Delaware Health Information Network
____________________________________ ____________________________________
[Name] Janice L. Lee, MD
[Title] Chief Executive Officer
Date: Date:







