DEPARTMENT OF HEALTH AND SOCIAL SERVICES
Division of Medicaid and Medical Assistance
PROPOSED
PUBLIC NOTICE
Title XXI Delaware Healthy Children Program State Plan - Premium Requirements
In compliance with the State's Administrative Procedures Act (APA - Title 29, Chapter 101 of the Delaware Code), 42 CFR §447.205, and under the authority of Title 31 of the Delaware Code, Chapter 5, Section 512, Delaware Health and Social Services (DHSS) / Division of Medicaid and Medical Assistance (DMMA) proposed to amend the Title XXI Delaware Healthy Children Program State Plan and the Division of Social Services Manual (DSSM) regarding Cost Sharing and Payment, specifically, Premium Requirements.
Any person who wishes to make written suggestions, compilations of data, testimony, briefs or other written materials concerning the proposed new regulations must submit same to: Planning, Policy and Quality Unit, Division of Medicaid and Medical Assistance, 1901 North DuPont Highway, P.O. Box 906, New Castle, Delaware 19720-0906, Attention: Kimberly Xavier; by email to Kimberly.Xavier@state.de.us, or by fax to 302-255-4425 by 4:30 pm on January 2, 2017. Please identify in the subject line: CHIP Premium Requirements.
The action concerning the determination of whether to adopt the proposed regulation will be based upon the results of Department and Division staff analysis and the consideration of the comments and written materials filed by other interested persons.
SUMMARY OF PROPOSAL
The purpose of this notice is to advise the public that Delaware Health and Social Services (DHSS)/Division of Medicaid and Medical Assistance (DMMA) is proposing to amend the Title XXI Delaware Healthy Children Program State Plan and the Division of Social Services Manual (DSSM) regarding Cost Sharing and Payment, specifically, Premium Requirements.
Statutory Authority
Background
The Balanced Budget Act of 1997, enacted on August 5, 1997, established the "State Children's Health Insurance Program (SCHIP)" by adding Title XXI to the Social Security Act. The purpose of this program is to provide funds to States to enable them to initiate and expand the provision of child health assistance to uninsured, low-income children in an effective and efficient manner that is coordinated with other sources of health benefits coverage for children. Delaware's SCHIP program called the Delaware Healthy Children Program (DHCP) is authorized under Title 19, Chapter 99, and Section 9905 of the Delaware Code.
Modified Adjusted Gross Income (MAGI) Conversion Plan
Under the Affordable Care Act, to complete the transition to the MAGI-based methodology, states developed MAGI-based income eligibility standards for the applicable eligibility groups that "are not less than the effective income levels" that were used to determine Medicaid and CHIP income eligibility as of the enactment of the Affordable Care Act. The conversion of current income eligibility standards to equivalent MAGI-based income eligibility standards account for any income disregards now used. Finally, under section 1902(e)(14)(E) of the Act, each state must submit to the Secretary for approval its proposed MAGI-equivalent income eligibility standards and the methodologies and procedures that support those proposed standards, for each applicable eligibility group. This submission is referred to as the state's "MAGI Conversion Plan". Delaware's conversion plan was approved on September 17, 2013.
The conversion to MAGI-based income eligibility standards impacts the percentages of the Federal Poverty Level (FPL) used to set the premium levels under CHIP. The Centers for Medicare and Medicaid Services (CMS) advised Delaware that the State needed to amend the Delaware's Children's Health Insurance Program (CHIP) State Plan to update the premium levels to account for the MAGI-based conversion standards. Therefore, Delaware Health and Social Services (DHSS)/Division of Medicaid and Medical Assistance (DMMA) drafted a proposed CHIP State Plan Amendment (SPA) to change the percentages of the Federal Poverty Level (FPL) applied to the premium levels and to describe the incentives for pre-payment of premiums. The proposed regulation was published in the September 2014 Delaware Register of Regulations for public comment. The final regulation was published in the November 2014 Delaware Register of Regulations and the SPA was submitted to CMS on December 17, 2014. DMMA worked with CMS over the course of two (2) years to re-work the language in Delaware's CHIP State Plan to reflect the new ACA requirements, and update the CHIP family premium cost sharing amounts to be consistent with the state's approved Modified Gross Income conversion plan. The SPA was approved on May 19, 2016.
Summary of Proposal
Effective July 1, 2014, CHIP families have been required to pay monthly premiums according to federal poverty level (FPL) as detailed below:
1. The ten dollar ($10.00) per family per month premium for families with incomes between 101% and 133% of the Federal Poverty Level (FPL) is obsolete. Children in these families transitioned to Medicaid effective January 1, 2014.
2. The conversion to MAGI-based standards results in a premium of fifteen dollars ($15.00) per family per month for families with incomes ranging from 143% to 176% of the FPL, and $25 PFPM for families with incomes ranging from 177% to 212% of the FPL (refer to CHIP MAGI State Plan Page CS21 for information on the effect of non-payment of premiums). This was a change from the originally a premium of fifteen dollars ($15.00) per family per month for families with incomes between 134% and 166% of the FPL and a premium of twenty-five dollars ($25.00) per family per month for families with incomes between 167% and 212% of the FPL that was proposed in September 2014.
Section 8 of the DHCP State Plan and Section 18700 of the Division of Social Services Manual (DSSM) have been amended to reflect the above-referenced change to the premium levels.
In addition, based on agency review, DHSS/DMMA amended the DHCP state plan at section 8.2.1 to update the language regarding incentives for pre-payment of premiums. The updated language reflects incentives for pre-payment of premiums that have been in practice since the inception of Delaware's CHIP program. These incentives are described at Section 18700 of the Division of Social Services Manual (DSSM).
The following regulations show the changes from the final version that was published in the December 2014 Register to those that CMS approved on May 19, 2016.
Public Notice
In accordance with the federal public notice requirements established at Section 1902(a)(13)(A) of the Social Security Act and 42 CFR 447.205 and the state public notice requirements of Title 29, Chapter 101 of the Delaware Code, Delaware Health and Social Services (DHSS)/Division of Medicaid and Medical Assistance (DMMA) gives public notice and provides an open comment period for thirty (30) days to allow all stakeholders an opportunity to provide input regarding these required changes made at the direction of the Center for Medicare and Medicaid Services (CMS). Comments must be received by 4:30 p.m. on January 2, 2017.
Centers for Medicare and Medicaid Services Review and Approval
The provisions of this state plan amendment (SPA) have been approved by the Centers for Medicare and Medicaid Services (CMS). The draft SPA page(s) have undergone further revisions since the initial publication as a result of CMS feedback and thus is being republished.
Provider Manuals Update
Also, upon CMS approval, the applicable Delaware Medical Assistance Program (DMAP) Provider Policy Specific Manuals will be updated. Manual updates, revised pages or additions to the provider manual are issued, as required, for new policy, policy clarification, and/or revisions to the DMAP program. Provider billing guidelines or instructions to incorporate any new requirement may also be issued. A newsletter system is utilized to distribute new or revised manual material and to provide any other pertinent information regarding manual updates. DMAP provider manuals and official notices are available on the DMAP website: http://www.dmap.state.de.us/home/index.html
Fiscal Impact
These regulations are being published to share changes made as a result of CMS feedback and direction. Current practice is not changing. Therefore, there is no fiscal impact.
DMMA REGULATION #16-028a
REVISION:
MODEL APPLICATION TEMPLATE FOR
STATE CHILD HEALTH PLAN UNDER TITLE XXI OF THE SOCIAL SECURITY ACT
STATE CHILDREN'S HEALTH INSURANCE PROGRAM
DELAWARE HEALTHY CHILDREN PROGRAM
Section 8. Cost Sharing and Payment (Section 2103(e))
Check here if the state elects to use funds provided under Title XXI only to provide expanded eligibility under the state’s Medicaid plan, and continue on to Section 9.
8.1. Is cost-sharing imposed on any of the children covered under the plan? (42 CFR 457.505)
8.1.1. YES
8.1.2. NO, skip to question 8.8.
Describe the amount of cost-sharing and any sliding scale based on income, the group or groups of enrollees that may be subject to the charge and the service for which the charge is imposed or time period for the charge, as appropriate. (Section 2103(e)(1)(A)) (42CFR 457.505(a), 457.510(b) & (c), 457.515(a)&(c))
8.2.1. Premiums: Fifteen dollars ($15.00) per family per month for families with incomes between 134% and 166% ranging from 143% to 176% of the Federal Poverty Level (FPL) and twenty-five dollars ($25.00) per family per month for families with incomes between 167% and 212% ranging from 177% to 212% of the FPL See Section 4.3 and (refer to CHIP MAGI State Plan Page CS21 for information on the effect of non-payment of premiums).
Incentives for pre-payment of premiums include the following: Pay three (3) months get one (1) premium free month; pay six (6) months get two (2) premium free months; pay nine (9) months get three (3) premium free months.
DMMA REGULATION #16-028a
REVISION:
8.5 Describe how the State will ensure that the annual aggregate cost-sharing for a family does not exceed 5 percent of such family's income for the length of the child's eligibility period in the State. Include a description of the procedures that do not primarily rely on a refund given by the State for overpayment by an enrollee: Section 2103(e)(3)(B)) (42CFR 457.560(b) and 457.505(e))
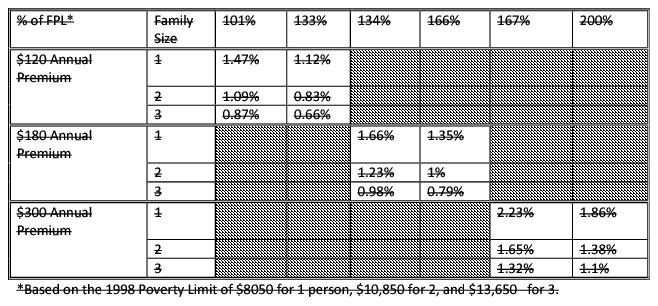
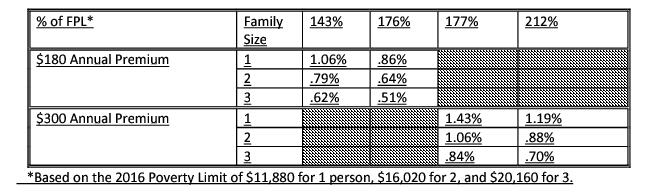
Since cost sharing is per family per month (PFPM), rather than per member per month, each family will pay the same amount no matter the number of children in the household. The premium rates are significantly less than those allowed by the Balance Budget Act of 1997 for premiums (see chart below). There is a minimal copayment of $10 per inappropriate use of the emergency room that will be waived if a prudent layperson would deem the visit an emergency or if it results in an inpatient admission. Delaware believes these levels of cost sharing are affordable but, at the same time, provide an incentive for clients to responsibly use health care services and avoid unnecessary emergency room visits.
An analysis of the State's fee schedule suggests that cumulative cost-sharing will rarely exceed 1% of the family's adjusted gross income. However, should families submit evidence that they have reached the aggregate limit on cost-sharing, the State will work with the MCOs on an individual basis to exempt the family from future cost-sharing.
Premiums as a percentage of Income
DMMA REGULATION #16-028b
REVISION:
Families with eligible children are required to pay a premium in order to receive coverage. The premium is per family per month regardless of the number of eligible children in the family. The monthly premium will vary according to family income as follows:
Family Income | Premium |
134% FPL = 176% FPL | $15.00 |
177% FPL = 212% FPL | $25.00 |
Family Income | Premium |
≥ 143% ≤ 176% | $15.00 |
≥ 177% ≤ 212% | $25.00 |
Payments that are less than one (1) month’s premium will not be accepted.
Coverage begins the first of the month following payment of the initial premium. Payments for the initial premium will be accepted through a monthly cut-off date known as the authorization date. The authorization date is set by the automated eligibility system. If payment of the initial premium is received by the authorization date, coverage under DHCP will be effective the following month. Premium payments for ongoing coverage will be accepted through the last day of the month.
Families will be able to pay in advance and purchase up to one year’s coverage. The following incentive is offered for advance payments:
Pay three (3) months – get one (1) premium free month
Pay six (6) months – get two (2) premium free months
Pay nine (9) months – get three (3) premium free months.
The advance premium payments for coverage may extend beyond the scheduled eligibility renewal. If the child is determined to be ineligible, the advance premium payments will be refunded to the family.
Coverage will be cancelled when the family is in arrears for two premium payments. The coverage will end the last day of the month when the second payment is due. If one premium payment is received by the last day of the cancellation month, coverage will be reinstated.
Families who lose coverage for nonpayment of premiums will have received two unpaid months of coverage. Families who are cancelled for nonpayment of premiums may reenroll at any time without penalty. Reenrollment will begin with the first month for which the premium paid.
Good cause for nonpayment of premiums will be determined on a case-by-case basis.







