department of health and social services
Division of Medicaid and Medical Assistance
PROPOSED
PUBLIC NOTICE
Medicaid Recovery Audit Contractor Program
In compliance with the State's Administrative Procedures Act (APA - Title 29, Chapter 101 of the Delaware Code) and under the authority of Title 31 of the Delaware Code, Chapter 5, Section 512, Delaware Health and Social Services (DHSS) / Division of Medicaid and Medical Assistance (DMMA) is amending the Title XIX Medicaid State Plan to comply with section 6411 of the Affordable Care Act regarding the Medicaid Recovery Audit Contractor Program.
Any person who wishes to make written suggestions, compilations of data, testimony, briefs or other written materials concerning the proposed new regulations must submit same to Sharon L. Summers, Planning & Policy Development Unit, Division of Medicaid and Medical Assistance, 1901 North DuPont Highway, P.O. Box 906, New Castle, Delaware 19720-0906 or by fax to 302-255-4425 by December 31, 2010.
The action concerning the determination of whether to adopt the proposed regulation will be based upon the results of Department and Division staff analysis and the consideration of the comments and written materials filed by other interested persons.
SUMMARY OF PROPOSAL
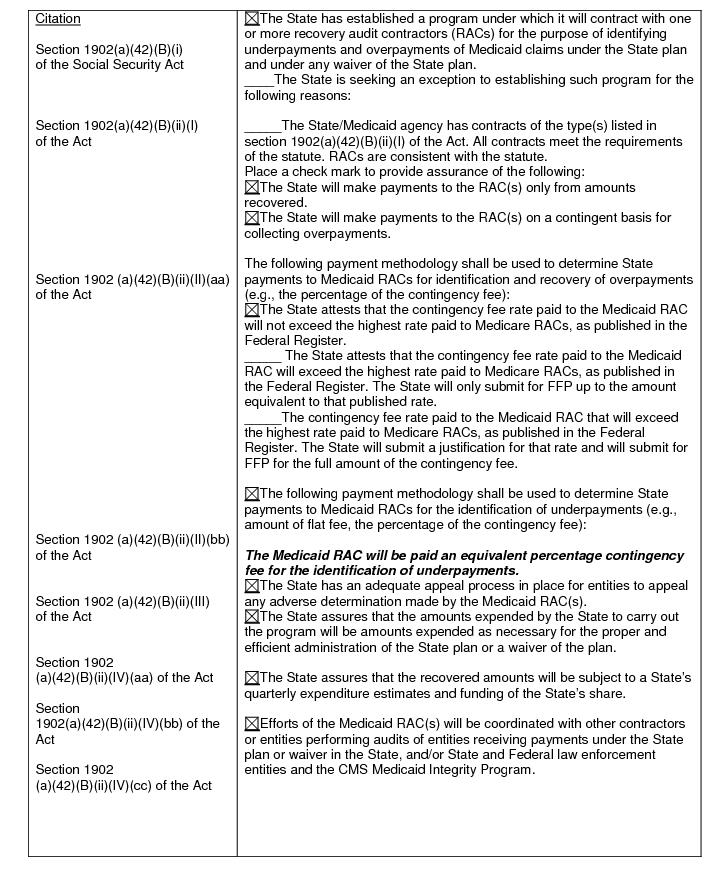
The proposal amends the Title XIX Medicaid State Plan to comply with section 6411 of the Affordable Care Act which amends section 1902(a)(42) of the Social Security Act (the Act) requiring States to establish programs to contract with RACs to audit payments to Medicaid providers by December 31, 2010.
Statutory Authority
The Patient Protection and Affordable Care Act, Public Law 111-148, Section 6411, Expansion of the Recovery Audit Contractor (RAC) program.
Background
State Medicaid RACs
Under Section 1902(a)(42)(B)(i) of the Act, States and Territories are required to establish programs to contract with one or more Medicaid RACs for the purpose of identifying underpayments and overpayments and recouping overpayments under the State plan and under any waiver of the State plan with respect to all services for which payment is made to any entity under such plan or waiver. States must establish these programs in a manner consistent with State law, and generally in the same manner as the Secretary contracts with contingency fee contractors for the Medicare RAC program.
The Centers for Medicare and Medicaid Services (CMS) will allow States to maintain flexibility in the design of Medicaid RAC program requirements and the number of entities with which the States elect to contract within the parameters of the statutory requirements. There are a number of operational and policy considerations in State Medicaid RAC program design (some of which will be discussed in greater depth in future rulemaking) such as:
a. Qualifications of Medicaid RACs;
b. Required personnel - for example physicians and certified coders;
c. Contract duration;
d. RAC responsibilities;
e. Timeframes for completion of audits/recoveries;
f. Audit look-back periods;
g. Coordination with other contractors and law enforcement;
h. Appeals; and
i. Contingency fee considerations.
Contingency Fees
Sections 1902(a)(42)(B)(ii)(I) and (II) of the Act provide that payments to Medicaid RACs are to be made only from amounts “recovered” on a contingent basis for collecting overpayments and in amounts specified by the State for identifying underpayments. CMS will not dictate contingency fee rates, but will establish a maximum contingency rate for which Federal Financial participation (FFP) will be available. This rate will be the highest contingency fee rate that is paid by CMS under the Medicare RAC program.
Appeals
Section 1902(a)(42)(B)(ii)(III) of the Act requires States to have an adequate process for entities to appeal any adverse decisions made by the Medicaid RACs. Each State has existing administrative appeals processes with respect to audits of Medicaid providers. So long as States are able to accommodate Medicaid RAC appeals within their existing Medicaid provider appeal structure, CMS is not requiring States to adopt a new administrative review infrastructure to conduct Medicaid RAC appeals.
Reporting
States will be required to report to CMS their contingency fee rates, along with other Medicaid RAC contract metrics such as the number of audits conducted, recovery amounts, number of cases referred for potential fraud, contract periods of performance, contractors’ names, and other factors such as whether a State has implemented provider or service-specific Medicaid RACs. States will report certain elements of this information via the quarterly Form CMS-64, and other information via separate data reporting forms CMS will require.
Coordination
Section 1902(a)(42)(B)(ii)(IV)(cc) of the Act requires that CMS ensure that States and their Medicaid RACs coordinate their recovery audit efforts with other entities.
Summary of Proposal
In accordance with the statutory requirements of Section 6411 of the Affordable Care Act, the Division of Medicaid and Medical Assistance (DMMA) intends to submit a State plan amendment (SPA) through which Delaware will attest that it will establish a compliant Medicaid RAC program by December 31, 2010.
State programs to contract with Medicaid RACs are not required to be fully operational by December 31, 2010. However, CMS expects States to fully implement their RAC programs by April 1, 2011.
The provisions of this state plan amendment are subject to approval by the Centers for Medicare and Medicaid Services (CMS).
Fiscal Impact Statement
This revision imposes no increase in cost on the General Fund; however, there is the potential for administrative and system change costs.
DMMA PROPOSED REGULATION #10-51
REVISION: