DEPARTMENT OF HEALTH AND SOCIAL SERVICES
Division of Medicaid and Medical Assistance
PROPOSED
PUBLIC NOTICE
Asset Verification System
In compliance with the State's Administrative Procedures Act (APA - Title 29, Chapter 101 of the Delaware Code), 42 CFR §447.205, and under the authority of Title 31 of the Delaware Code, Chapter 5, Section 512, Delaware Health and Social Services (DHSS) / Division of Medicaid and Medical Assistance (DMMA) is proposing to amend Title XIX Medicaid State Plan regarding the Asset Verification System, specifically, to identify the contractor selected to implement the system.
Any person who wishes to make written suggestions, compilations of data, testimony, briefs or other written materials concerning the proposed new regulations must submit same to, Planning, Policy and Quality Unit, Division of Medicaid and Medical Assistance, 1901 North DuPont Highway, P.O. Box 906, New Castle, Delaware 19720-0906, by email to Nicole.M.Cunningham@state.de.us, or by fax to 302-255-4413 by 4:30 p.m. on August 31, 2018. Please identify in the subject line: Asset Verification System.
The action concerning the determination of whether to adopt the proposed regulation will be based upon the results of Department and Division staff analysis and the consideration of the comments and written materials filed by other interested persons.
SUMMARY OF PROPOSAL
The purpose of this notice is to advise the public that Delaware Health and Social Services (DHSS)/Division of Medicaid and Medical Assistance (DMMA) is proposing to amend Title XIX Medicaid State Plan regarding the Asset Verification System, specifically, to identify the contractor selected to implement the system.
Statutory Authority
Background
In a letter dated February 8, 2012, CMS approved DE SPA# 11-011 which proposed to implement an Asset Verification System, a system for verifying the assets of aged, blind or disabled applicants for and recipients of Medicaid.
Individuals whose eligibility is being determined or redetermined (and others whose finances are relevant to eligibility) must authorize the State agency to obtain records from any financial institution in connection with the eligibility determination in order to verify the individual's assets. The verification program is to be "consistent with the approach of the Commissioner of Social Security" under Section 1631 of the SSA, i.e., an electronic verification system. Individuals who refuse or revoke their authorization may be determined ineligible for medical assistance.
For purposes of implementing an asset verification program under this section, a State may select and enter into a contract with a public or private entity. The DE SPA# 11-011 did not identify a contractor.
Although Delaware has been complying with and meeting the requirements of AVS, in an effort to provide increased efficiency and oversite, a Request for Proposal was issued in 2017 and a contractor identified.
Summary of Proposal
Purpose
The purpose of this proposed regulation is to identify the contractor selected to implement the Asset Verification System.
Summary of Proposed Changes
Effective for services provided on and after October 1, 2018 Delaware Health and Social Services/Division of Medicaid and Medical Assistance (DHSS/DMMA) proposes to amend Title XIX Medicaid State Plan pages Supplement 16 to Attachment 2.6 A Pages 1 - 3 regarding the Asset Verification System, specifically, to identify the contractor selected to implement the system.
Public Notice
In accordance with the federal public notice requirements established at Section 1902(a)(13)(A) of the Social Security Act and 42 CFR 447.205 and the state public notice requirements of Title 29, Chapter 101 of the Delaware Code, Delaware Health and Social Services (DHSS)/Division of Medicaid and Medical Assistance (DMMA) gives public notice and provides an open comment period for thirty (30) days to allow all stakeholders an opportunity to provide input on the proposed regulation. Comments must be received by 4:30 p.m. on August 31, 2018.
Centers for Medicare and Medicaid Services Review and Approval
The provisions of this state plan amendment (SPA) are subject to approval by the Centers for Medicare and Medicaid Services (CMS). The draft SPA page(s) may undergo further revisions before and after submittal to CMS based upon public comment and/or CMS feedback. The final version may be subject to significant change.
Provider Manuals and Communications Update
Also, there may be additional provider manuals that may require updates as a result of these changes. The applicable Delaware Medical Assistance Program (DMAP) Provider Policy Specific Manuals and/or Delaware Medical Assistance Portal will be updated. Manual updates, revised pages or additions to the provider manual are issued, as required, for new policy, policy clarification, and/or revisions to the DMAP program. Provider billing guidelines or instructions to incorporate any new requirement may also be issued. A newsletter system is utilized to distribute new or revised manual material and to provide any other pertinent information regarding DMAP updates. DMAP updates are available on the Delaware Medical Assistance Portal website: https://medicaid.dhss.delaware.gov/provider
Fiscal Impact
The following fiscal impact is projected:
|
|
Federal Fiscal Year 2018
|
Federal Fiscal Year 2019
|
|
Federal funds
|
$570,906
|
$217,536
|
|
General (State) funds
|
$91,137
|
$72,512
|
AMENDED Supplement 16 to Attachment 2.6-A
Page 1
STATE PLAN UNDER TITLE XIX OF THE SOCIAL SECURITY ACT
STATE/TERRITORY: DELAWARE
ASSET VERIFICATION SYSTEM
|
1940(a)
|
1. The Agency will provide for the verification of assets for purposes of determining or redetermining Medicaid eligibility for aged, blind and disabled Medicaid applicants and recipients using an Asset Verification System (AVS) that meets the following minimum requirements.
A. The request and response system must be electronic:
(1) Verification inquiries must be sent electronically via the internet or similar means from the Agency to the financial institution (FI).
(2) The system cannot be based on mailing paper-based requests.
(3) The system must have the capability to accept responses electronically.
B. The system must be secure, based on a recognized industry standard of security (e.g., as defined by the U.S. Commerce Department's National Institute of Standards and Technology, or NIST).
C. The system must establish and maintain a database of FIs that participate in the Agency's AVS.
D. Verification requests also must be sent to FIs other than those identified by applicants and recipients, based on some logic such as geographic proximity to the applicant's home address, or other reasonable factors whenever the Agency determines that such requests are needed to determine or redetermine the individual's eligibility.
E. The verification requests must include a request for information on both open and closed accounts, going back up to 5 years.
|
|
TN No. SPA 18-026
TN No. SPA 11-011
|
Approval Date
Effective Date July 1, 2018
|
AMENDED Supplement 16 to Attachment 2.6 A
Page 2
STATE PLAN UNDER TITLE XIX OF THE SOCIAL SECURITY ACT
STATE/TERRITORY: DELAWARE
ASSET VERIFICATION SYSTEM
TN No. SPA 18-026 TN No. SPA 11-011 | Approval Date Effective Date July 1, 2018 |
AMENDED Supplement 16 to Attachment 2.6 A
Page 3
STATE PLAN UNDER TITLE XIX OF THE SOCIAL SECURITY ACT
STATE/TERRITORY: DELAWARE
ASSET VERIFICATION SYSTEM
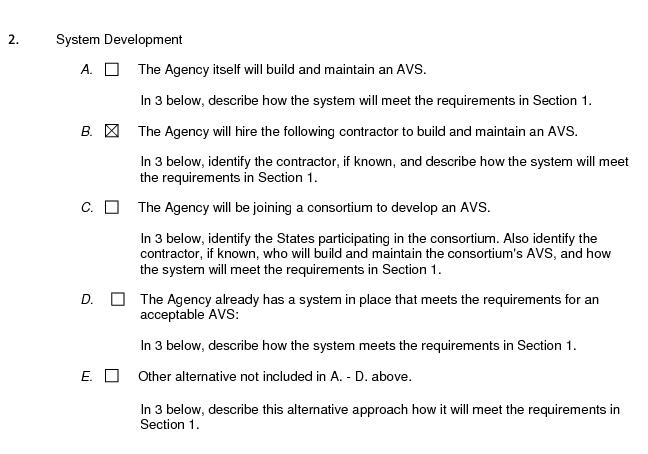
2. Provide the AVS implementation description and other information requested for the implementation approach checked in Section 2.
The contractor is not known at this time.
The Agency will select a contractor through the Request for Proposal (RFP) process.
Delaware has contracted with Public Consulting Group Incorporated to provide an Asset Verification System (AVS), to identify assets of Medicaid applicants and recipients held at various Financial Institutions (FI’s). This system complies The system and entity chosen will be able to comply with the following requirements of Supplement 16 to Attachment 2.6-A, Page 1:
A. An electronic request and response process for asset verification;
B. A database of financial institutions (FIs) that provide data to the entity meeting the geographic
requirements of the entity;
C. A 5-year look-back of the assets on individual applicants, recipients, spouses and partners;
D. A secure system based on a recognized industry standard as defined by the United States
Commerce Department's National Institute of Standards and Technology, or NIST;
E. Verification request will include both open and closed asset account information as determined by
the State;
F. The acceptable asset verification entity will provide adequate data for the generation of all required
reports expected to meet federal reporting requirements such as the number of requests, number
of responses and amounts of undisclosed assets found.
TN No. SPA 18-026 TN No. SPA 11-011 | Approval Date Effective Date July 1, 2018 |







